Abstract
- The diffuse cerebellar dysfunction as a permanent neurological sequela of or-ganophosphate poisoning has not yet been reported in the published literature. We report a diffuse cerebellar dysfunction as a permanent manifestation of or-ganophosphate poisoning. A 55-year-old man diagnosed with acute organophos-phate poisoning was brought to the emergency room of our hospital. He had slurred, monotonous scanning speech with irregularly distributed articulatory deficits, and prominent bilateral limb ataxia. He presented left-beating spontaneous nystagmus with a downbeat component and strong downbeating nystagmus after head shaking. He also showed saccadic hypometria with a normal saccadic velocity at fixed horizontal saccades and symmetrically impaired horizontal smooth pursuit on both sides. The poisoning of organophosphate poisoning may lead to a diffuse permanent cerebellar dysfunction as a neurological sequela event.
-
Keywords: Organophosphate poisoning; Cerebellar dysfunction; Case reports
INTRODUCTION
Organophosphate, a potent acetylcholinesterase inhibitor, is a frequent cause of substance intoxication [1,2]. The spectrum of neurological manifestations of organophosphate poisoning in the chronological manners from the standpoint of the evolution of symptoms including the initial cholinergic phase with miosis, depressed mental status, and seizure, the intermediate syndrome with a myasthenia syndrome-like proximal muscle weakness, and the delayed symptoms such as encephalopathy, extrapy-ramidal syndrome and axonal polyneuropathy, has been pre-viously reported [1–4]. However, there were no prior reports on diffuse cerebellar dysfunction as a permanent defect of organo-phosphate poisoning. We experienced a patient with diffuse cerebellar dysfunction as a permanent manifestation of organo-phosphate poisoning.
CASE REPORT
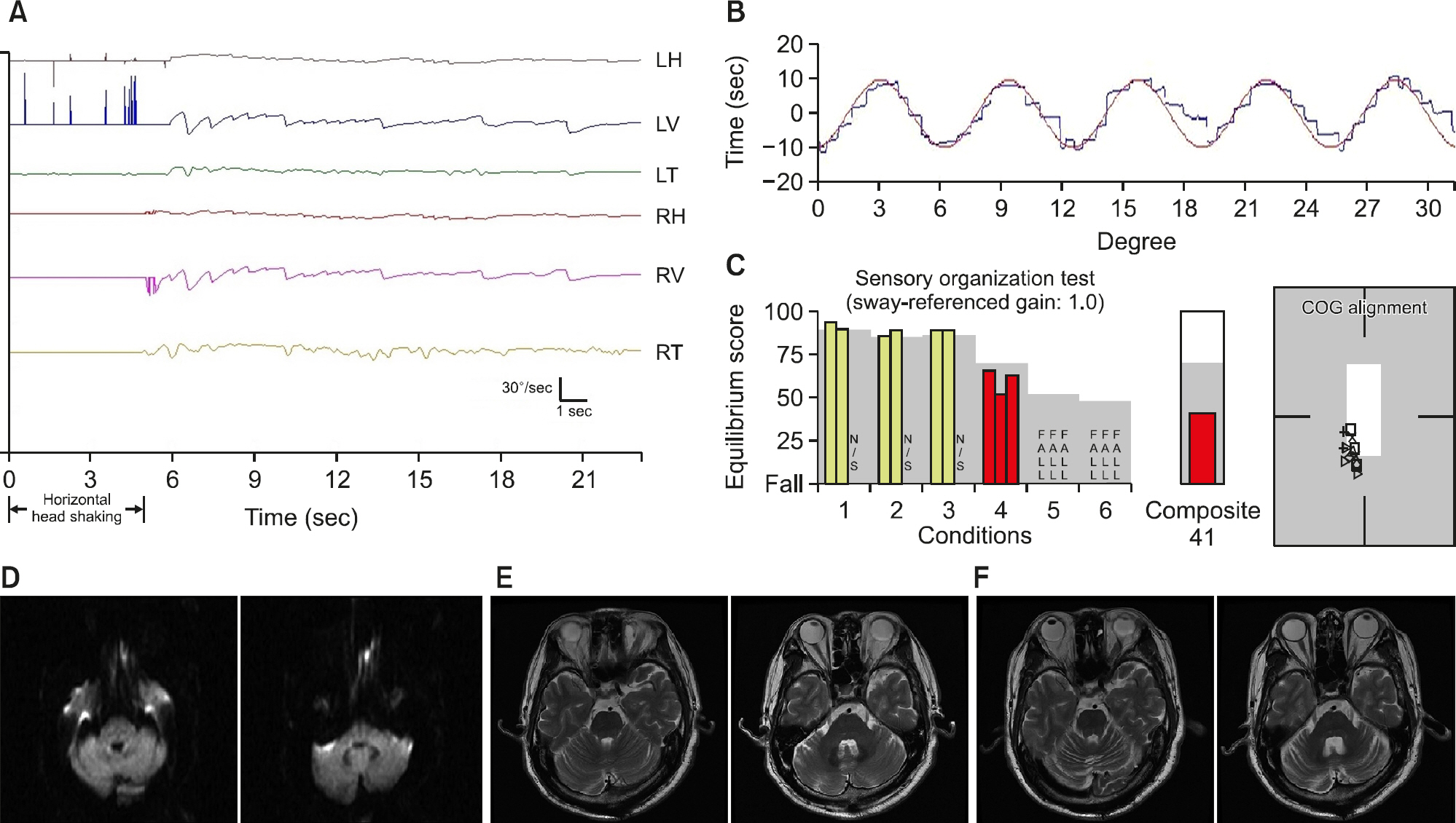
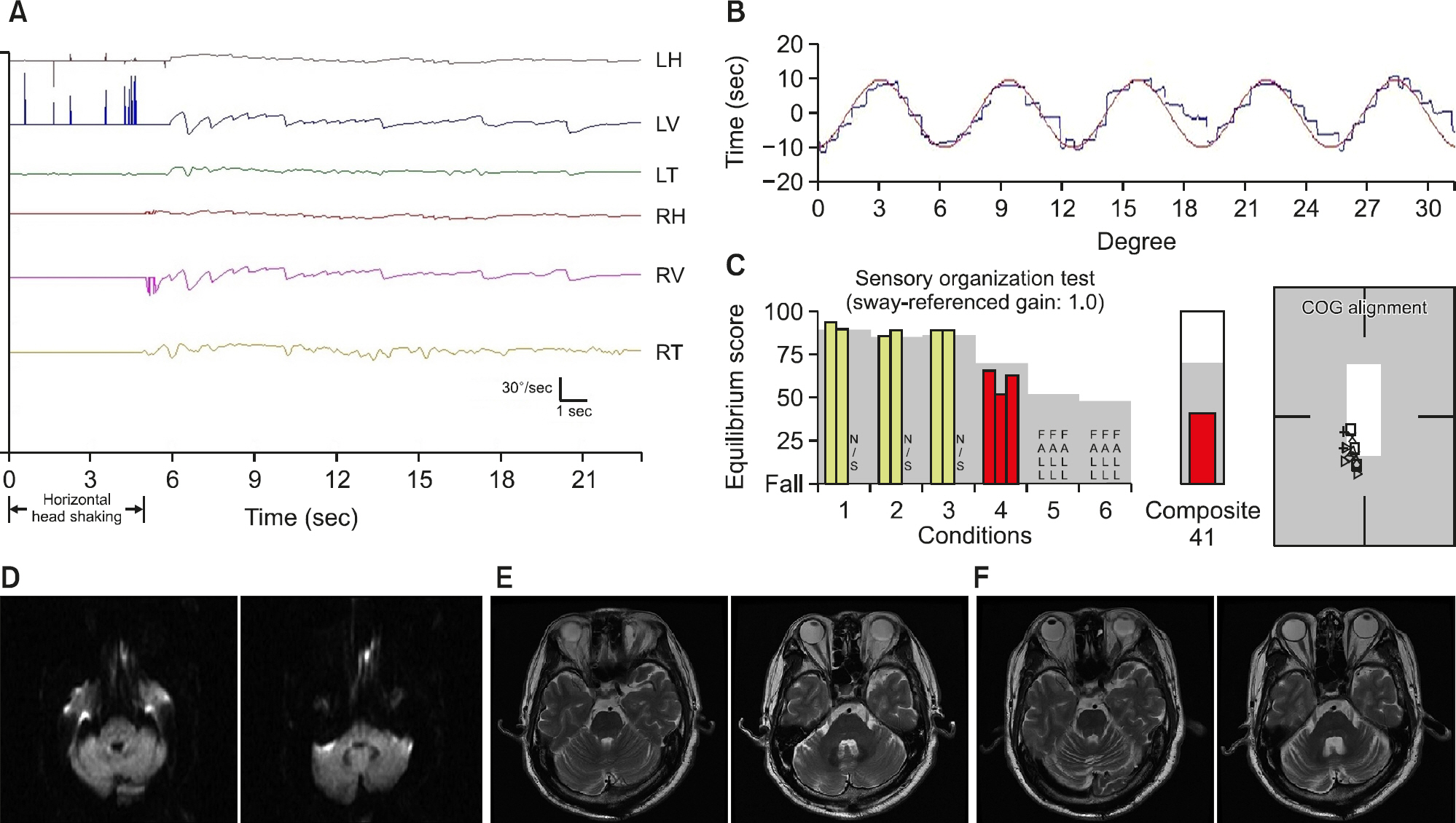
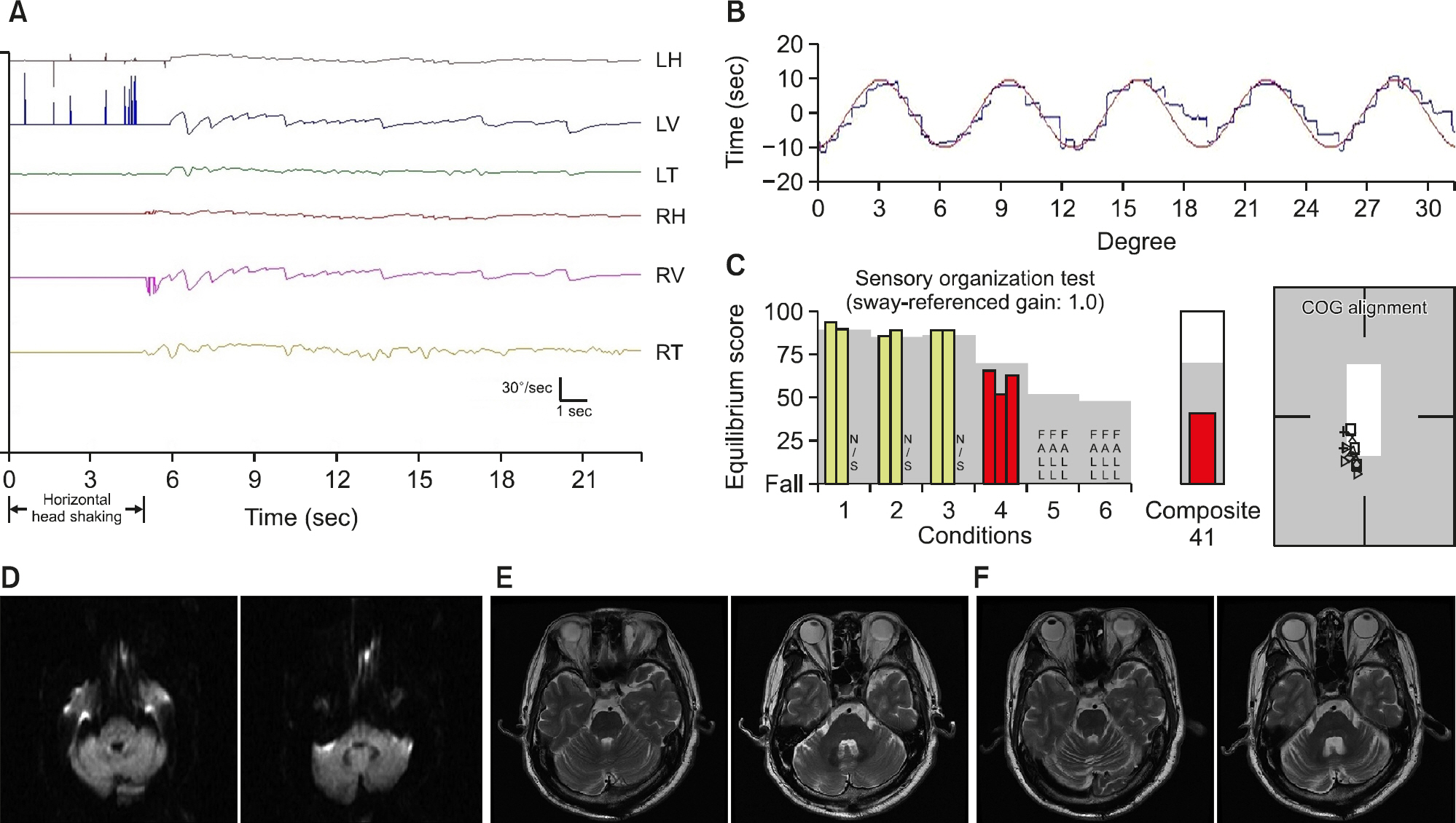
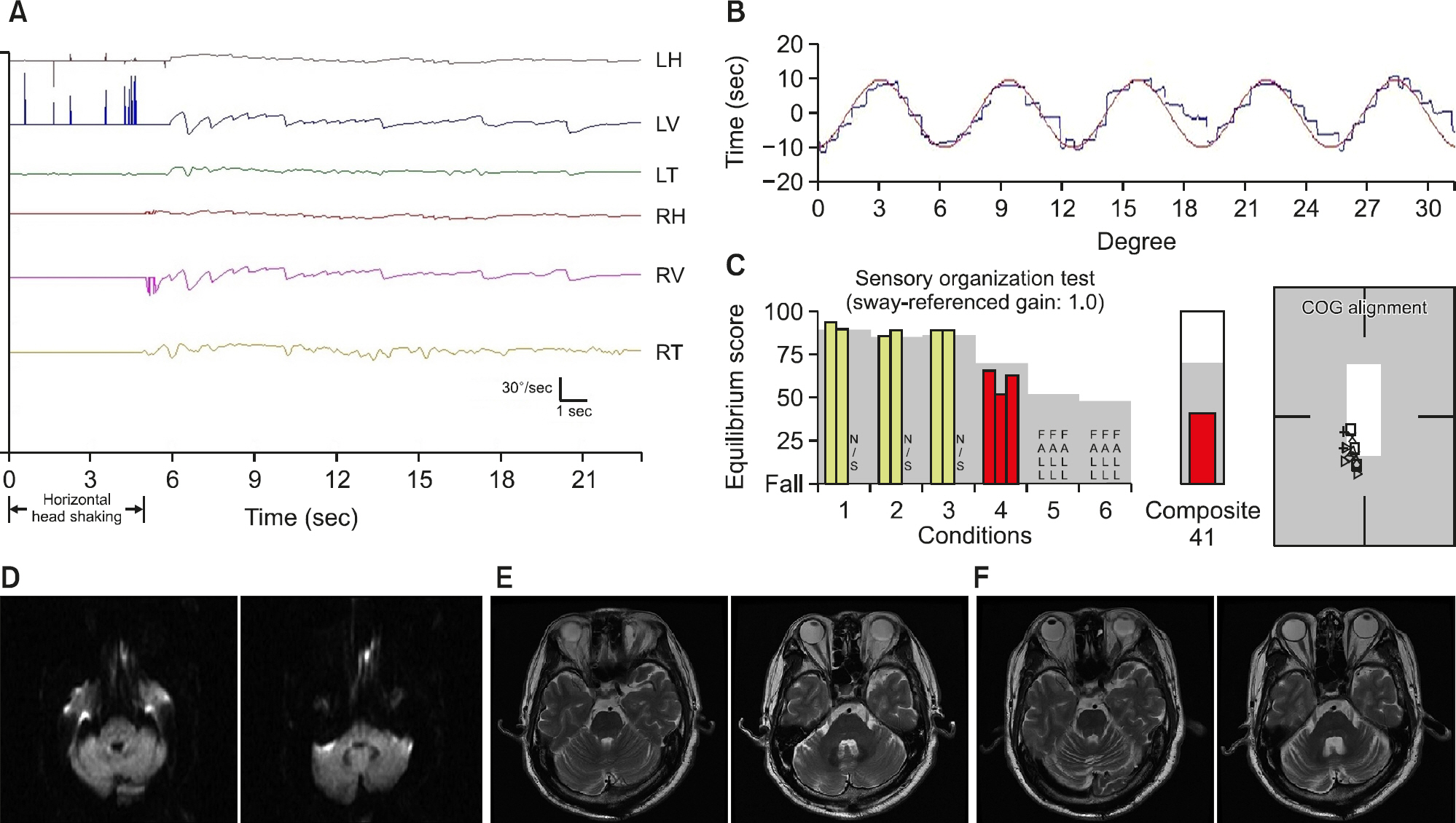
A 55-year-old man was referred to our hospital due to mental change. He was social alcoholics and did not take any medi-cations. He drank a bottle containing organophosphate pesti-cides for suicide. He lost his consciousness, but he recovered his mentality after gastric lavage and charcoal application at the previous hospital. After several hours, he lost consciousness again and was transferred to our hospital. At arrival, he was drowsy and intubated. Arterial blood gas analysis was within a normal range. Serum pseudocholinesterase level was 161 U/L (normal range for men, 3,500–11,400 U/L). Pralidoxime chloride and atropine were administered intravenously to reduce the excessive cholinergic effect. With 10 days of ventilator care, he recovered self-breathing and consciousness. Fifteen days after admission, he noticed dysarthria, dizziness, and clumsiness of his both hands. On neurological examination, he had slurred, monotonous scanning speech with irregularly distributed arti-culatory deficits, and prominent bilateral limb ataxia. He could stand without support, but could not walk independently. Other neurological examinations were normal. Video-oculography (SensoMotoric Instruments, Teltow, Germany) testing showed left-beating spontaneous nystagmus with a downbeat component and strong downbeating nystagmus (27°/sec) after head shaking (Fig. 1A). In oculomotor testing, saccadic hypometria with a normal saccadic velocity at fixed horizontal saccades and sym-metrically impaired horizontal smooth pursuit on both sides (Fig. 1B) were observed. Computerized dynamic posturography showed severe vestibular deficit with falling to the backward when the visual and proprioceptive inputs were interrupted (Fig. 1C). Bithermal caloric stimulation showed a normal response. Diffusion-weighted (Fig. 1D) brain magnetic resonance imaging (MRI) performed on the admission day and T2-weight images (Fig. 1E) on 15 days after organophosphate poisoning were unremarkable, but follow-up T2-weight brain MRI taken after 10 months showed diffuse cerebellar atrophy (Fig. 1F). His symptoms were slowly improved over several months, but un-steadiness, dysarthria, and clumsiness of both hands were per-sistent on the last follow-up (10 years after symptoms). The patient showed saccadic hypometria and impaired horizontal smooth pursuit on both sides, bilateral gaze-evoked nystagmus and downbeating head-shaking nystagmus at the 10-year follow-up.
Fig. 1.(A) After horizontal head shakings for 5 seconds, strong downbeat nystagmus with a maximal velocity of 27°/sec is shown. A small component of left-beating nystagmus is also seen. (B) Horizontal smooth pursuit test (10°/sec, 0.2 Hz) showed symmetrically impaired saccadic pursuit on both sides. (C) Sensory organization test in computerized dynamic posturography showed a severe vestibular deficit with falling when the visual and proprioceptive inputs were interrupted (e.g., conditions 5 and 6; sway-referenced gain: 1.0). In all conditions, the center of gravity (COG) alignment tended to be tilted to the backward. Diffusion-weighted images (D) of first brain magnetic resonance imaging (MRI) performed on the day of organophosphate poisoning, and axial T2-weighted images performed 15 days after onset of symptoms (E) showed no abnormalities in the cerebellum. Ten months later, the axial T2-weighted image of follow-up MRI (F) showed diffuse cerebellar atrophy. LH, left horizontal; LV, left vertical; RH, right horizontal; RV, right vertical; RT, right torsional.
The study was approved by the Institutional Review Board of Keimyung University Dongsan Medical Center (No. 2020-09-005). Written informed consent was waived due to its retro-spective nature.
DISCUSSION
We observed diffuse and permanent cerebellar dysfunction as a prominent symptom in a patient with acute organophos-phate poisoning. Two prior reports [3,4] described a patient with acute organophosphate poisoning who lately developed cerebellar ataxia as a delayed neurological sequela. However, in those reports, imaging such as MRI was not addressed at the time of cerebellar dysfunction, and the lesion may be limited to an area responsible for cerebellar ataxia. Furthermore, previous reports did not include oculographic data, which is an essential tool for evaluating the eye movement and balance function that is commonly impaired in the cerebellar lesion.
The damage to the central vestibular structure, including ves-tibulocerebellum, is most likely responsible for perverted head- shaking nystagmus with a normal caloric response in our patient. Cerebellar dysarthria is usually localized to the paravermal segments of the rostral cerebellar hemisphere [5], and sym-metrically impaired smooth pursuit is known to be associated lesion in the dorsal oculomotor vermis [6]. The lesion responsible for limb dysmetria is commonly localized to the rostral lateral cerebellar hemisphere, which is known to be related predominantly to limb control [7]. The severe gait ataxia with falling in our patient has mostly been ascribed to lesions in the rostral vermis, which is related to gait and postural control [7]. In view of neurological symptoms and signs, cerebellar dysfunction in our patient may result from injury to broad areas of the cerebellum, including the vestibulocerebellum, bilateral cerebellar hemispheres, rostral vermis, dorsal oculomotor ver-mis, and paravermal segments of the rostral cerebellar hemi-sphere.
The cerebellum is known to be a frequent target organ of various toxic agents [8]. Purkinje or granular cell layers of the cerebellum are also known as an area preferentially susceptible to ischemic or toxic encephalopathy [8]. Without pathological confirmation, it is difficult to know the pathomechanism on how organophosphate causes neurological defects preferentially involving the cerebellum. However, considering the previous observation [8] that the neurotoxic effect of trichlorfon, one of the many organophosphate compounds, and its active metabolite dichlorvos can be mainly seen in the cerebellum through meth-ylation of DNA in the granular cell lays, it is reasonably as-sumed that organophosphate in pesticides drank in our patient may cause a toxic effect to the granular cell lays of the ce-rebellum preferentially by methylation of DNA and inhibition of its cell repair mechanism, which finally leads to neuronal cell death.
Hypoxic-ischemic encephalopathy could not be excluded as a cause of cerebellar damage in our patient. The cerebellum can show the damage that is often limited to the watershed zones in mild cases of hypoxic-ischemic brain injury and can be widespread in severe cases. Cerebellar Purkinje fibers are hypermetabolic and, therefore, sensitive to hypoxic injury [8,9]. In the acute stage (less than 24 hours) of hypoxic-ischemic injury, cytotoxic edema makes a high signal in diffusion-weighted images and corresponding low signal on apparent diffusion coefficient map in brain MRI [9]. However, diffusion-weighted images of the admission day and T2-weight images of brain MRI performed on 15 days after organophosphate poisoning showed no signal change. Because he recovered his mentality after gastric lavage and charcoal and lost consciousness again inside the hospital, we could assume the period of hypoxia might be short. Also, arterial blood gas analysis was within the normal range at the time of change in mentality. Accordingly, we presume that organophosphate intoxication itself is more reasonably considered as a cause of diffuse cerebellar dys-function in our patient than acute hypoxic-ischemic brain injury.
중심 단어: 유기인산염 중독, 소뇌 기능 장애, 증례보고
CONFLICT OF INTEREST
Dr. Lee serves on the editorial boards of the Research in Vestibular Science, Frontiers in Neurology: Neuro-otology, and Current Medical Imaging Review. No other potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Rusyniak DE, Nañagas KA. Organophosphate poisoning. Semin Neurol 2004;24:197–204.ArticlePubMed
- 2.Peter JV, Sudarsan TI, Moran JL. Clinical features of organophosphate poisoning: A review of different classification systems and approaches. Indian J Crit Care Med 2014;18:735–45.ArticlePubMedPMC
- 3.Michotte A, Van Dijck I, Maes V, D'Haenen H. Ataxia as the only delayed neurotoxic manifestation of organophosphate insecticide poisoning. Eur Neurol 1989;29:23–6.Article
- 4.Fonseka MM, Medagoda K, Tillakaratna Y, Gunatilake SB, de Silva HJ. Self-limiting cerebellar ataxia following organophosphate poisoning. Hum Exp Toxicol 2003;22:107–9.ArticlePubMed
- 5.Urban PP, Marx J, Hunsche S, Gawehn J, Vucurevic G, Wicht S. Cerebellar speech representation: lesion topography in dysarthria as derived from cerebellar ischemia and functional magnetic resonance imaging. Arch Neurol 2003;60:965–72.ArticlePubMed
- 6.Takagi M, Zee DS, Tamargo RJ. Effects of lesions of the oculomotor cerebellar vermis on eye movements in primate: smooth pursuit. J Neurophysiol 2000;83:2047–62.ArticlePubMed
- 7.Sohn SI, Lee H, Lee SR, Baloh RW. Cerebellar infarction in the territory of the medial branch of the superior cerebellar artery. Neurology 2006;66:115–7.ArticlePubMed
- 8.Fonnum F, Lock EA. Cerebellum as a target for toxic substances. Toxicol Lett 2000;112-113:9–16.ArticlePubMed
- 9.White ML, Zhang Y, Helvey JT, Omojola MF. Anatomical patterns and correlated MRI findings of non-perinatal hypoxic-ischaemic encephalopathy. Br J Radiol 2013;86:20120464. ArticlePubMedPMC
Citations
Citations to this article as recorded by






 KBS
KBS
 PubReader
PubReader ePub Link
ePub Link Cite
Cite