특징적안진이 없는 양성돌발성두위현훈 의심환자에서 어지럼 및 심리척도
Dizzy and Psychological Scales in Benign Paroxysmal Positional Vertigo: Suspicious Patients without Characteristic Nystagmus
Article information
Trans Abstract
Objectives
Patients, who have had a history of benign paroxysmal positional vertigo (BPPV)-like symptoms, but no characteristic nystagmus, were often present. They are diagnosed as having a resolved state from BPPV or normal, and tend to be overlooked. We investigated the dizzy and psychological scales in BPPV-suspicious patients.
Methods
Thirty-nine patients, which they had vertigo of a short duration at the specific head position, and clinically suspicious BPPV, but no nystagmus in positional tests, were enrolled. We compared dizzy and psychological scales of suspicious BPPV patients with 138 BPPV patients, using dizziness handicap inventory (DHI), the beck depression inventory (BDI), and the Spielberger state-trait anxiety inventory. Additionally, among the BPPV-suspicious group, patients with a BPPV history were compared with those with no previous BPPV.
Results
No differences in the all scales were found between the two groups. However, DHI scores of patients with a previous BPPV attack were significantly higher than those of patients with no BPPV-like symptoms; in particular, there was a significant difference in emotional scores.
Conclusion
Although the patients had no characteristic nystagmus, if they have a BPPV-like history and symptoms, emotional support and periodic follow up are needed. In particular, careful observation should be performed in patients with previous BPPV attack.
INTRODUCTION
Benign paroxysmal positional vertigo (BPPV) is one of the most frequent vestibular disorders. BPPV is known to be caused by detachment of the otoconia from the otolithic membrane of the utricle and a move into either the semicircular canal or the utricular side of the ampulla [1]. Thus, for diagnostic purposes of BPPV, the positioning nystagmus investigation enables localization of the side affected and that of the damaged canal [2]. Clinically, BPPV of the posterior canal is characterized by onset of torsional and up-beating nystagmus of short duration (30–60 seconds) with a latency of 7 to 8 seconds and vertigo symptoms of a paroxysmal nature in the Dix-Hallpike test. Additionally, for patients with lateral and anterior canals, characteristic nystagmus was observed, such as geotropic or ageotropic, and torsional and down-beating nystagmus, respectively, in the head-rolling and Dix-Hallpike test. Generally, patients with BPPV complain of the development of vertigo symptoms when they are turning onto one side, getting up abruptly, craning their head to take something off a high shelf, or during abrupt head movements [3].
However, we have often found patients who have a typical history of BPPV and vertigo symptoms but do not show any characteristic nystagmus. They did or did not demonstrate positional vertigo in the positional and positioning tests and showed anxiety about a severe vertigo attack. However, if they have normal vestibular function test findings and no other disorder that was able to cause the positional vertigo, they were mostly diagnosed as being in a resolved state from BPPV or as having normal vestibular function with no definite abnormality in the vestibular function test, and tend to be overlooked. We investigated the dizzy and psychological scales in these BPPV-suspicious patients, who have a typical history of BPPV but did not have positional nystagmus.
MATERIALS AND METHODS
The present prospective study, designed for patients with positional vertigo, was approved by the Institutional Review Board of Hallym University (IRB no., 2013-098). Patients with complaints of positional rotatory vertigo of short duration with a typical history of BPPV—the development of vertigo when they lie down in one direction, tilt their head back or turn their head in the supine position, accompanied by nausea or vomiting. Informed consent was obtained from the patients, and we excluded patients with central vertigo, history of previous psychological disorder, or suspicion of psychogenic dizziness.
All participants underwent a detailed diagnostic procedure consisting of clinical, neurological, and otological examinations. The vestibular function test included positional and positioning maneuvers, caloric test, pursuit, saccadic, optokinetic tests, vestibular evoked myogenic potentials, electrocochleography and auditory brainstem response. Additionally, audiological tests, a complete blood count and blood chemistry were performed. The patients, in whom no nystagmus was found and, in other tests, no remarkable findings were shown, were included in the present study. Thus, through their test findings and history, in them, no disease other than BPPV or BPPV-resolved state, could be considered.
Based on history and test results, 39 patients were diagnosed with suspicious BPPV. Of 39 patients, 22 patients experienced the BPPV-like symptoms for the first time, and 17 patients had had a previous BPPV attack, which were diagnosed as BPPV after neuro-otolgogic examination at the department of otolaryngology clinic.
Patients’ dizziness and psychological symptoms were also measured using the Korean versions of the dizziness handicap inventory (DHI), the beck depression inventory (BDI), and the Spielberger state-trait anxiety inventory (STAI). The Korean version of these scales is a translation of the original English sentences of these scales into Korean, so that patients could understand the questions, and there was no difference between them.
The DHI is a self-administered scale of self-perceived handicapping effects imposed by vestibular disease [4]. The BDI is a 21-item self-reported scale developed to measure depression symptoms. Response categories range from 0 (not at all) to 3 (very much). Summation of the results gives a BDI score ranging from 0 to 63. A score ≥21 is considered to indicate clinically relevant depression syndromes [5]. The STAI scale comprises four levels of anxiety intensity ranging from 1 (not at all) to 4 (very much), and the results are summed to give a score between 20 and 80. A cutoff score of 40 is normally used to indicate clinically significant symptoms reflecting a state of anxiety [6].
We examined the DHI, BDI, and STAI scores at the first visit; for comparison of these scores, in patients with BPPV (they had a typical history and characteristic nystagmus in the positional or positioning test), DHI, BDI and STAI scores were examined.
Additionally, among the BPPV-suspicious group, patients with a BPPV history were compared with those with no previous BPPV.
1. Data analysis
Independent t-test was performed to compare the BPPV-suspicious and BPPV groups, and the Mann-Whitney U-test was performed to compare patients with a previous BPPV and those without a previous BPPV attack (ver. 11.5; SPSS Inc., Chicago, IL, USA). A p-value less than 0.05 was deemed to indicate statistical significance.
RESULTS
The average ages of the patients in the BPPV-suspicious and BPPV groups were 46.5 and 49.6 years, respectively, and the male:female ratios were 11:28 and 34:104, respectively (Table 1).
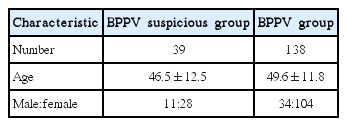
Demographics of BPPV suspicious patients group without characteristic nystagmus and BPPV patients group with characteristic nystagmus
No statistical differences were shown in DHI scores, including functional, emotional and physical subscales between the BPPV-suspicious and BPPV groups (Fig. 1). Additionally, regarding the BDI and STAI scores, no difference was observed (Fig. 2).

Comparison of dizziness handicap inventory (DHI) and subscales between the benign paroxysmal positional vertigo (BPPV)-suspicious and BPPV patient groups.
Comparison of beck depression inventory (BDI), and Spielberger state-trait anxiety inventory (STAI) scales between the benign paroxysmal positional vertigo (BPPV)-suspicious and BPPV patient groups.
However, among the BPPV-suspicious group, patients with a BPPV history presented significantly higher DHI scores than those without a BPPV history and, particularly with regard to emotional subscales, differences were observed (Fig. 3).
Comparison of dizziness handicap inventory (DHI) and subscales between the patients with a benign paroxysmal positional vertigo (BPPV) history and those without a BPPV history. *p<0.05.
BDI and STAI scores were higher in patients with a BPPV history than in those without a BPPV history, but there was no statistical difference (Fig. 4).
DISCUSSION
Between 17% and 42% of patients with vertigo ultimately receive a diagnosis of BPPV [7,8]. In patients with BPPV, debris (thought to be fragmented endolymph particles) entering the semicircular canal becomes “trapped” and causes inertial changes in the semicircular canal, thereby resulting in abnormal nystagmus and vertigo with head motion in the plane of the canal [1,9].
BPPV is diagnosed when (1) patients report a history of vertigo provoked by changes in head position and (2) when, on physical examination, characteristic nystagmus is provoked by the Dix-Hallpike maneuver or supine roll test [10].
Of the above diagnostic criteria of BPPV, we conducted the present study for patients with only a history of BPPV. We took a detailed history and performed vestibular function tests for exclusion of other vestibular diseases and enrolled BPPV-suspicious patients in the present study. Mostly, they were considered to be in a resolved state from BPPV spontaneously or to have normal vestibular function, and would not be considered for further management or observation.
Of course, various diseases such as vestibular neuritis, meniere’ disease, vestibular paroxysmia, perilymph fistula and vestibular migraine, can induce the positional vertigo, symptom of BPPV. But, in this study, we could exclude these diseases through detailed history, regular follow-up, vestibular function tests and consultation with other department.
We have found that BPPV-suspicious patients, with no characteristic nystagmus, have DHI scores and depression and anxiety scales similar to those of BPPV patients. Thus, we should know that they could be afflicted with vertigo or disequilibrium and have psychological distress such as depression and anxiety. Vestibular deficits are risk factors for the development of secondary psychiatric disorders [11], and a somatopsychic hypothesis has been suggested. Conversely, patients with psychiatric disorders often report dizziness as a concomitant phenomenon in their illness [12]. This linkage of vestibular and psychiatric symptoms in patients with dizziness is the subject of an ongoing debate [13]. Additionally, it was reported that the most important factor influencing the development of psychological distress in patients with vestibular disease is the severity of vertigo symptoms rather than the type of vestibular disease or other factors [14]. Thus, the severity of vertigo that patients have experienced during the attack could induce psychological distress in the BPPV and BPPV-suspicious patient groups.
Additionally, we found that patients with a previous BPPV attack have higher dizziness scores than patients with a first attack. This finding was attributed to the higher emotional subscale of DHI scores, although the depression and anxiety scales were not significantly different. In the case of a patient with a previous BPPV attack, the experience of severe vertigo symptoms in the past may function as a trigger for emotional instability.
Several probable hypotheses for BPPV-suspicious patients (who had a history of BPPV but did not have characteristic nystagmus in positional and positioning tests) could be suggested. First, they could have a minimum level of calcium carbonate particles, but not sufficient to cause nystagmus [15]. Second, an explanation for BPPV without nystagmus was proposed by Johkura et al. They perceived that, among elderly patients with dizziness, the sensitivity of conventional assessment using Frenzel goggles was low for the detection of nystagmus. Thus, it was possible that we had failed to detect present nystagmus [16]. Third, spontaneous resolution of BPPV could have occurred. It is known that most episodes of BPPV, even in untreated patients, recover spontaneously in 2 to 6 weeks. The major process involved in the spontaneous recovery of BPPV episodes is considered to be the capability of the endolymph to dissolve dislodged otoconia [17]. However, whatever may be the precise cause of the absence of nystagmus, it is thought that even if BPPV-suspicious patients do not show characteristic nystagmus, they should be monitored more closely. It is necessary to understand the discomfort that the patient has and to stabilize the patient's mind.
In conclusion, we have found that patients who were suspicious for BPPV, but without characteristic nystagmus, felt dizzy and had psychological distress in common with BPPV patients. It was thought that the patients were not in a state of absent sickness and, in the management of the patients, attention was paid to the dizziness and psychological distress; furthermore, particularly, for patients with previous BPPV, emotional support was necessary.
Notes
No potential conflict of interest relevant to this article was reported.