전정 발작에서 청성뇌간반응의 진단적 가치
Is the Auditory Brainstem Response Diagnostic for Vestibular Paroxysmia?
Article information
Trans Abstract
Objectives
Vestibular paroxysmia (VP) of the eighth cranial nerve is characterized by recurrent auditory and vestibular disturbances when a proximal part of the eighth cranial nerve is continuously pressed by a vessel. A detailed history and several ancillary diagnostic tools, such as tinnitogram, caloric test, auditory brainstem response (ABR) and magnetic resonance imaging, are used for diagnosis of VP. Among them, although Møller criteria using ABR is a simple method, the previous study is insufficient. Therefore, this study aimed to evaluate ABR’s diagnostic value of VP.
Methods
ABR records of the 14 patients (patient group) who were diagnosed with VP and 45 patients (as control) who were diagnosed with only tinnitus were reviewed retrospectively. We analyzed the differences in Møller criteria between 2 groups.
Results
Mean age of the patient group was 52.9 years old and the control group was 55.4 years old. As compared with the control group, there were no significant differences of Møller 3 criteria contents (peak II wave amplitude<33% [35.7% vs. 15.5%, p=0.133], interpeak latency I–III ≥2.3 msec [42.8% vs. 35.5%, p=0.622]), Contralateral interpeak latency III–V ≥2.2 msec (0% vs. 4.4%, p=1.000) in patient group.
Conclusion
There was no significant difference of ABR parameters according to the Møller criteria between patient and control groups.
INTRODUCTION
Vestibular paroxysmia (VP) of the eighth cranial nerve was first reported by Janetta in 1975 under the name of neurovascular compression syndrome (NVCS) and describes when a proximal part of the eighth cranial nerve in the cerebellopontine angle is continuously pressed by a vessel, resulting in repeated paroxysmal vertigo, tinnitus, or sensorineural hearing loss [1,2]. NVCS of the 8th cranial nerve was used in conjunction with the terms “disabling positional vertigo,” “vestibular paroxysmia” and “typewriter tinnitus” on the basis of the symptoms, all of which can be explained by the same mechanism [3,4] and is generally reported to occur more frequently in women in their 40s and 50s [5].
The major symptom is rotational vertigo lasting seconds to minutes in 63% of patients, and, in order of frequency, gait instability, nausea, vomiting, ipsilateral tinnitus, and aural fullness are also associated [3]. According to the pattern of symptoms, the diagnostic term and criteria of VP of the eighth cranial nerve have been adjusted and presented. The only confirmation for this disease requires surgical proof. Tests that are used to assist diagnosis include a tinnitogram, caloric test, auditory brainstem response (ABR) and magnetic resonance imaging (MRI) [6] Møller criteria using latency differences between the waves of ABR were published in 1990 and have been used to objectively diagnose this syndrome, but studies on the clinical value of ABR in VP have been scarce [7,8].
De Ridder et al. [8] reported that no ABR changes were detected during the first 2 years and that the prolongation of the ipsilesional interlatency I–III was related to the disease duration.
In this study, we analyzed whether Møller criteria are specific for VP and useful in clinical practice.
MATERIALS AND METHODS
From December 2012 to April 2016, ABR data of 14 patients diagnosed with definite VP at Hallym University Hospital were reviewed retrospectively. Patients who met the diagnostic criteria for definite VP according to the consensus document of the Committee for the Classification of Vestibular Disorders of the Barany Society were included (Table 1) [9].
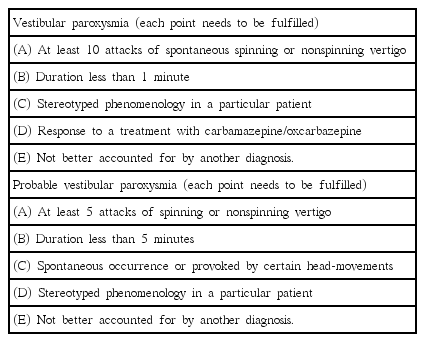
Diagnostic criteria for vestibular paroxysmia according to the consensus document of the Committee for the Classification of Vestibular Disorders of the Barany Society
All patients had repetitive paroxysmal attacks of vertigo and tinnitus and showed dramatic response to anticonvulsant medication.
In the same period, 45 patients who visited with continuous tinnitus and corresponding to normal hearing range of pure-tone average (0.5, 1, 2, and 3 kHz) were selected as controls, and their ABR results were compared to those of the patient group. The exclusion criteria of the control group included tinnitus that disturbed daily living or sleep, history of hearing loss or dizziness, otologic infections such as otitis media, ototoxic drug, acoustic trauma and ABR abnormality suggesting lesions in the cerebellopontine angle such as vestibular schwannoma and meningioma.
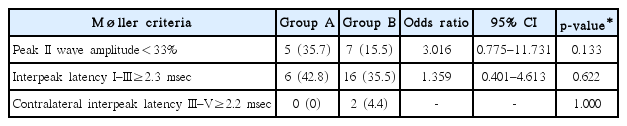
Based on the results of ABR, numbers corresponding to each of the three Møller criteria (interpeak latency I–III ≥2.3 msec, contralateral interpeak latency III–V ≥2.2 msec, and peak wave II amplitude<33%) were compared between patients and controls (Table 2).
The comparison of the 2 groups was analyzed with chi-square tests, Fisher exact test, and odds ratios. Statistical analysis was performed using IBM SPSS Statistics ver. 22.0 (IBM Co., Armonk, NY, USA). The study protocol was approved by the Institutional Review Board of the Hallym University Sacred Heart Hospital (approval number: 2017-I094).
RESULTS
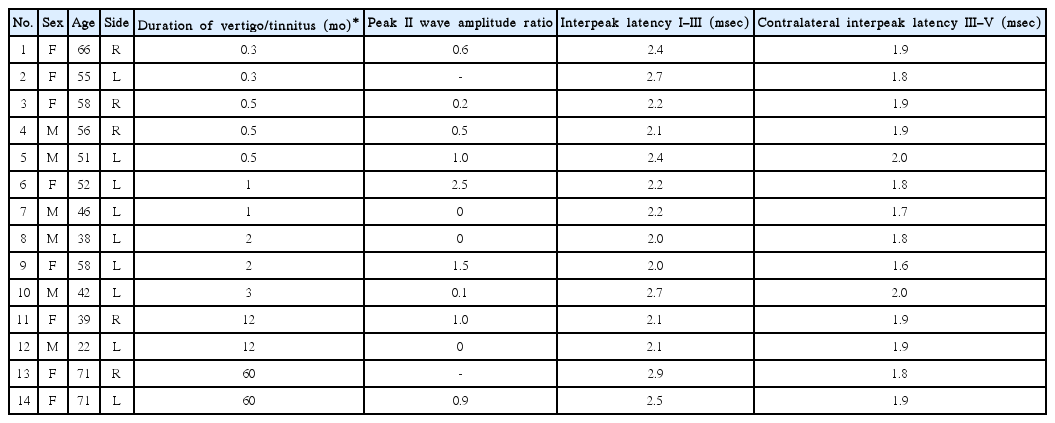
The mean age of the patient group was 51.8 years (range, 22–71 years), and that of the control group was 55.4 years (range, 19–68 years). Six of the 14 patients and 24 of the 45 controls were male patient. The mean duration of vertigo/tinnitus of patient group was 11.1 months (range, 0.5–60 months) (Table 3).
None of the comparisons of the 3 items of Møller criteria showed significant differences between the 2 groups. Here, 35.7% of the patients and 15.5% of the controls had a peak II wave amplitude<33% (p=0.133). Furthermore, 42.8% of the patients and 35.5% of the controls had an interpeak latency I-III ≥2.3 msec (p=0.622). In addition, none of the patients and 4.4% of controls had a contralateral interpeak latency III–V ≥2.2 msec (p=1.000) (Table 4).
DISCUSSION
Because the eighth cranial nerve is composed of a complex of auditory and vestibular nerves, symptoms of VP vary depending on the areas in which the vascular structure presses the nerve. Various combinations of auditory and vestibular symptoms are suggestive of this disease. While confirmation of neurovascular contact is only possible with a surgical procedure, a combination of characteristic symptoms and responsiveness to anticonvulsants has been used for diagnostic criteria in clinics [9]. Because of this, several tests (pure tone audiometry, tinnitogram, caloric test, MRI, ABR, etc.) are used to assist diagnosis. Among patients with this syndrome, 47% of them have been reported to have abnormal pure tone
audiometry results, and 28% of them complain of tinnitus [3]. As hearing decreases, tinnitus tends to worsen, and the pulsatile or typewriter type of tinnitus can help diagnose the syndrome [3,4,10]. Additionally, the caloric test shows that 33%–62% of patients suffering from VP have canal paralysis. Over time, the unilateral vestibular paralysis worsens [3].
The relationship between the eighth cranial nerve in the cerebellopontine angle and the vessel compressing the nerve can be identified radiologically by using the constructive interference in steady state (CISS) MRI technique [6,11]. The most common artery causing nerve compression has been reported to be the anterior inferior cerebellar artery, followed by the posterior inferior cerebellar artery. Rarely, the vertebral artery and small arteries and veins are also known to be involved [12-14]. Using the CISS MRI, Hüfner et al. [3] have found nerve compression by vascular structure in 95% of patients with VP.
The characteristics of ABR in the VP are as follows. According to the pathophysiology of microvascular compression of the proximal part of the eighth cranial nerve, there is a decrease or disappearance of the amplitude of wave II and the interlatency delay of wave I–III of the affected side and the interlatency delay of wave III–V of the contralateral side [7].
In the early phase of vascular compression, there is no change in ABR, but the amplitude of wave II is thought to decrease, and tinnitus occurs due to signal transmission failure after approximately 2 years. After 4 years, the signaling rate decreases due to local demyelination of the nerve and the interlatency of wave I–III is prolonged. Furthermore, the hearing of the frequency part where the tinnitus appears decreases. The extension of wave III–V on the normal side is assumed to be due to the slowing of the signal transmission in the brainstem to compensate for the interlatency delay of wave I–III on the affected side [8].
In this study, there was no significant difference in the 3 Møller criteria values between the patient and control groups.
Considering the relatively short duration of the disease in our subjects, this negative finding corresponds to the previously published study [8]. Because of the paroxysmal and repetitive nature of the symptoms, patients often show fearful responses and seek urgent medial relief. A valid tool for the objective diagnosis of this pathology would help make medical decisions regarding beginning anticonvulsant trials, despite the possibility of serious side effects. ABR is noninvasive and easy to perform.
Since Møller report in 1990, this test has been included in some diagnostic criteria [3]. However, the results of this study revealed that a negative ABR cannot rule out the possibility of the disease, again stressing the importance of recording a detailed history. We assumed that there would be a significant difference in ABR between the patients and control group over at least 2 years of observation. Nevertheless, the odds ratio for peak II wave amplitude <33% was 3.016, and this criterion seem to be worthy of diagnosis the disease in patients with shorter duration symptoms.
This NVCS is better known in the fifth (trigeminal neuralgia) and ninth (glossopharyngeal neuralgia) cranial nerves. The eighth cranial nerve is composed of the auditory nerve and vestibular nerve, and the facial nerve is in close proximity.
Therefore, VP may present with various symptoms. The site at which the blood vessel compresses the nerve is known as the central nervous segment, and the length of the central nervous segment of each cranial nerve has been reported to correlate with the frequency of the disease [15]. In other words, the anatomical location of each cranial nerve and blood vessels and the length of the central nerve segment of the cranial nerves may influence symptom expression [16].
In conclusion, VP can only be demonstrated surgically; therefore, the diagnosis depends on subjective symptoms, response to anticonvulsants and ancillary tests. The results of our study suggest that ABR in the diagnosis of VP cannot be an absolute criterion, but a decrease in the amplitude of wave II is considered to be a supplementary indicator to help in the diagnosis.
Notes
No potential conflict of interest relevant to this article was reported.
Acknowledgements
This work was supported by National Research Foundation of Korea (NRF) grants funded by the Korean Government (NRF-2016R1A2B4016330 and NRF-2013R1A1A3006802).