요가 후 발생한 양성돌발두위현훈
Benign Paroxysmal Positional Vertigo after Yoga Practice
Article information
Trans Abstract
A 57-year-old woman presented with sudden onset of whirling vertigo associated with nausea and vomiting. The neurological examination showed left-beating horizontal nystagmus on the lying-down test and right-beating horizontal nystagmus on the head bending test. Geotropic direction-changing horizontal nystagmus was demonstrated on both sides during the supine roll test. Benign paroxysmal positional vertigo (BPPV) was the most common vestibular disorder in patients after head trauma. The authors experienced a case of right horizontal canal BPPV occurred after a yoga practice, thereby we report the case with a review of the related literatures.
INTRODUCTION
Benign paroxysmal positional vertigo (BPPV) is the most common cause of peripheral vertigo, with a yearly incidence of 0.6% [1]. The provoked situations are lying down, tipping the head up or down, sitting up from a supine position, particularly after awaking in the morning, or turning over in bed. In addition, a reaction can be elicited by the patient looking upward, for example, to place an object on a shelf above the head, or bending forward to tie shoelaces. The majority of patients experience one or more seconds of latency following the movement before experiencing violent attacks of vertigo lasting 10–30 seconds and linear-rotatory nystagmus: the fast phase beating toward the undermost ear, or upward when the gaze is directed to the uppermost ear [2].
In several publications based on large numbers of BPPV cases, the cause of otoconial detachment could not be established in 34%–66% of idiopathic or primary BPPV cases, such as in elderly patients [3]. Although some scanning electron microscopy studies have found otoconia to have degenerated, more than one explanation of BPPV is possible, even in elderly patients [4]. The most common causes of acquired or secondary form of BPPV are thought to be head and labyrinth trauma, inner ear diseases such as viral neuro-labyrinthitis or vestibular neuritis, Meniere’s disease, vestibulobasilar ischemia and anterior inferior cerebellar artery syndrome, or prolonged bed rest due to unrelated disease. Occasionally BPPV is experienced following general surgery or procedures on the inner ear, such as stapes surgery [3,4]. In addition, it has been reported that minor head injuries cause BPPV even if they do not accompany any serious neurological abnormality or brain damage [5].
The authors had experienced a case of right horizontal canal BPPV occurred after a yoga practice, thereby we report this case with a review of the related literatures.
CASE REPORT
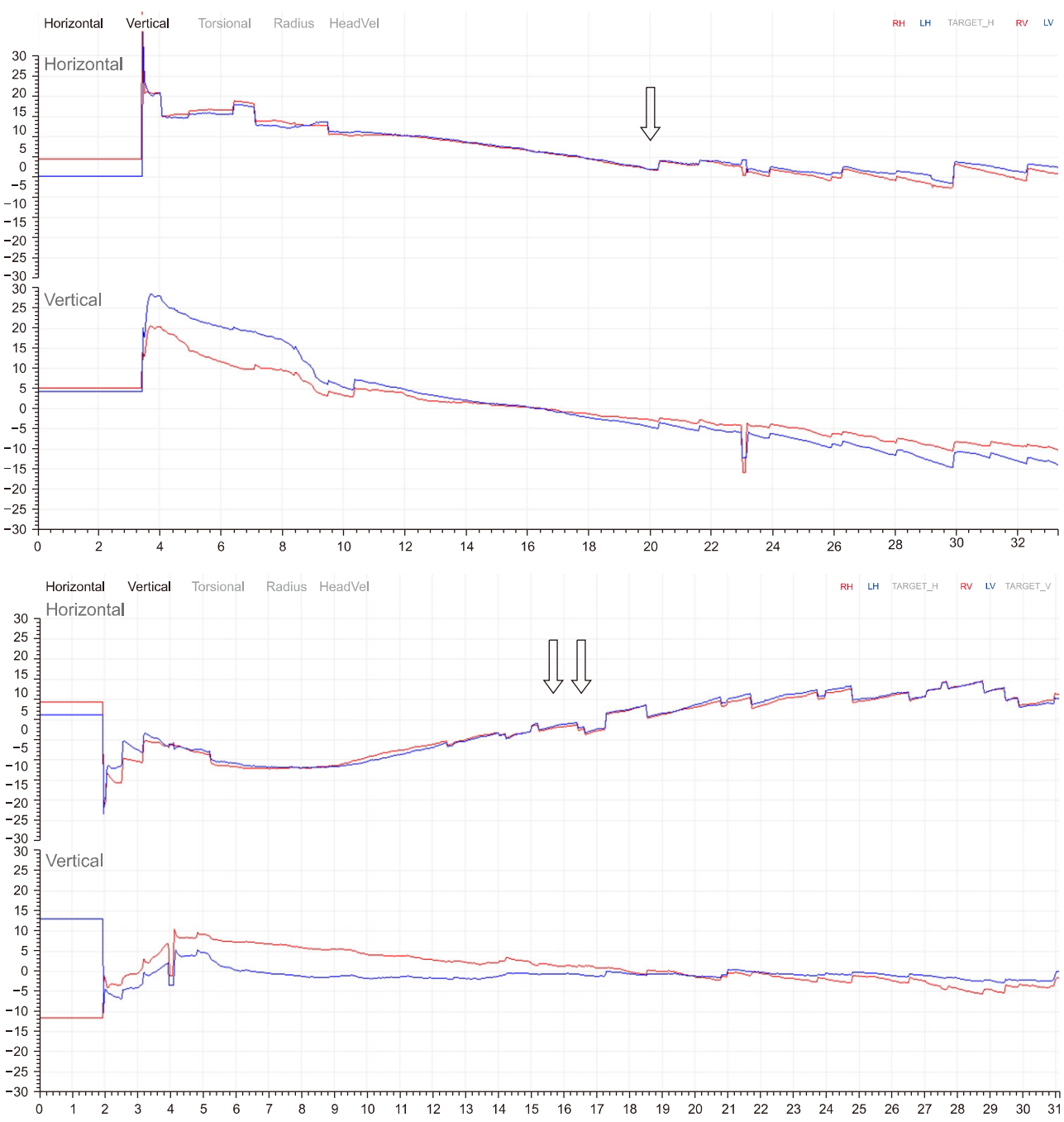
A 57-year-old woman presented with sudden onset of whirling vertigo for the first time in her life associated with nausea and vomiting from 1 day ago. The symptom of vertigo was mainly caused by sudden head movements and repetitive, and if not moving, improved about a few minutes later. She denied having tinnitus, aural fullness, hearing impairment, and diplopia. Her past medical history was unremarkable. Recently, she had been practiced the yoga over 1 hour a day during the latest one week. She said that the she had symptoms after her head in a crawling posture and then bowing her head again, so called “cat posture.” The results of standard laboratory analyses, and her neurological examination were within normal limits. Her oculomotor examination was normal. No spontaneous nystagmus was observed. there were no abnormal findings from the brain magnetic resonance imaging and magnetic resonance angiography. Video nystagmography (VNG) showed left-beating horizontal nystagmus on the lying-down test and right-beating horizontal nystagmus on the head bending test (Fig. 1). Bilateral geotropic direction-changing horizontal nystagmus was demonstrated on both sides during the supine roll test (Fig. 2). Authors diagnosed as canalolithiasis of right horizontal semicircular canal, a Barbecue rotation was performed to the patient. After repositioning procedure, the patient reported improvement of vertigo gradually. Also repetitive VNG showed decreased amplitude and duration of bilateral geotropic nystagmus. At the follow-up visit after one week from the treatment, there was no symptomatic recurrence. After discharge, she stopped practicing yoga.
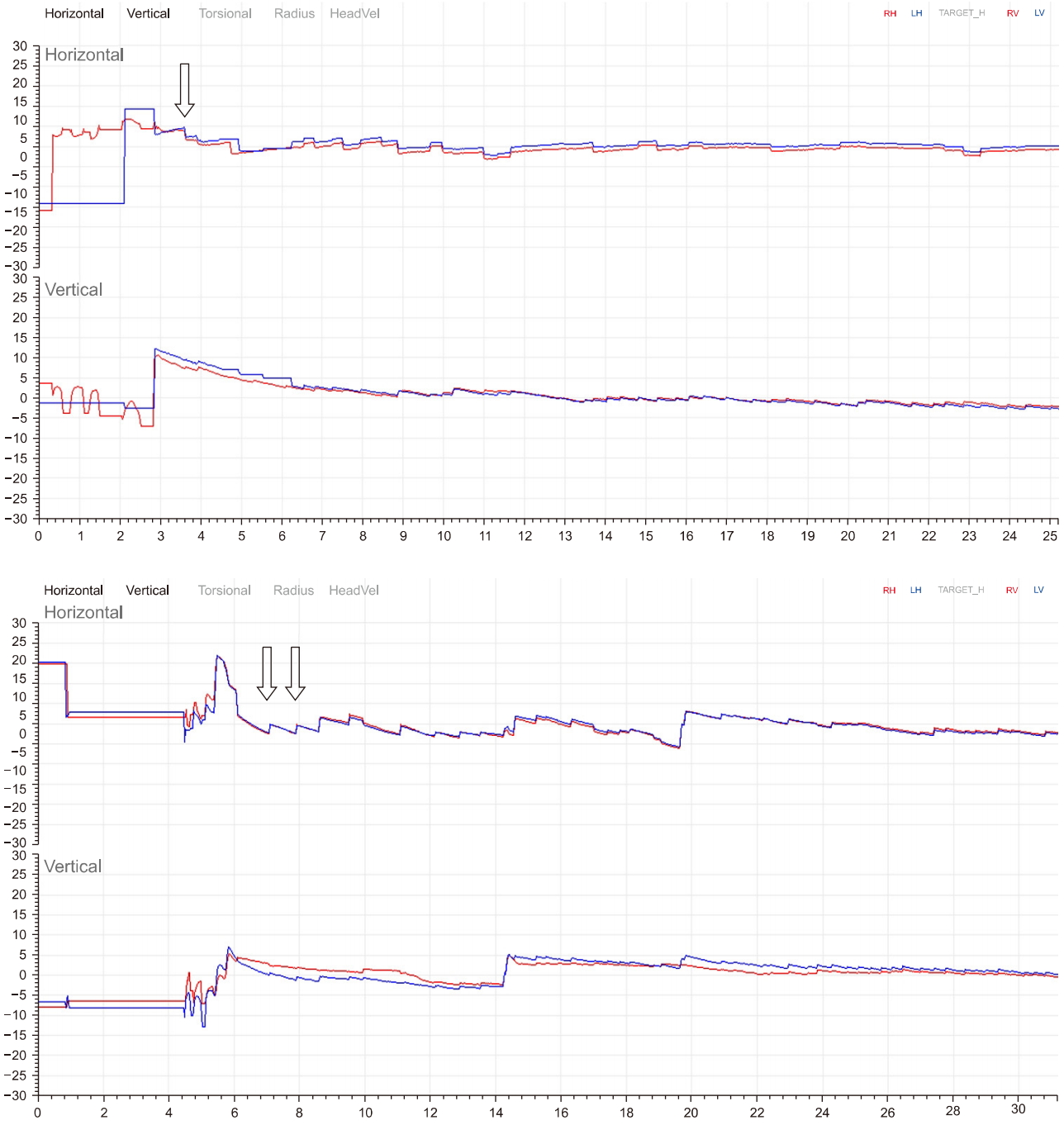
Video nystagmography showed left-beating horizontal nystagmus on the lying-down test (↓) and right-beating horizontal nystagmus on the head bending test (↓↓).
DISCUSSION
Yoga is a representative mind-body therapy of complementary and alternative medicine. Yoga has been reported to improve various stress-induced complaints of the mind and body, including anxiety, insomnia, and fatigue. The mechanism is gradually being elucidated regarding how yoga improves these symptoms [6]. However, reports on yoga-associated adverse events have also been increasing. These injuries include whiplash, muscle damage, back strain and neurological symptoms including vertigo. In addition, serious conditions such as stroke can also occur. Black has been warning people practicing yoga regarding these adverse effects of yoga [7]. According to one study, the second most common symptoms were of the nervous system, which was reported by 237 attendees (9.4%) [6]. These neurological symptoms were dizziness in 101 attendees (4.0%) and faintness in 33 attendees (1.3%).
Many authors found that BPPV was the most common vestibular disorder in patients after head trauma [8]. The onset typically appears just after trauma, or a few days or weeks after minor traumatic brain injury, and can be unilateral or bilateral. Even mild head injury could result in the detachment of otoconia in the endolymph. The cat posture is bowed and quickly lifted up, and the head moves more than 90°. This can give the head a shock similar to that caused by a car accident. Schuknecht discussed the pathogenetic aspects of posttraumatic BPPV. He proposed that head trauma, such as cat posture, which requires patient to raise her head quickly may disrupt the utricular otolith membrane, which may subsequently lead to a displacement of utricular otoconia into the semicircular canal, free to settle in the posterior or/and in the other canals, resulting in posttraumatic BPPV [9]. Accordingly, posttraumatic BPPV may be the result of the occurrence of multiple otoconial debris. Posttraumatic development of BPPV can also occur as the result of a degenerative process following labyrinth concussion, where after some time, an otoconial clump will accumulate, which could flow to an inappropriate site in the inner ear [3].
The incidence, duration, frequency, and intensity of BPPV symptoms vary, perhaps due to the frequent occurrence of spontaneous recovery. Katsarkas [10] identified posttraumatic etiology in 6.2% of 1,644 BPPV patients. Baloh et al. [11] noted the presence of BPPV in 240 patients, and attributed this to traumatic head injury in 17%. Hoffer et al. [8] identified BPPV in 29% of patients complaining of moderate and severe head trauma. Such variability in BPPV diagnosis could be attributable to differences in inclusion criteria, variability in the patients who need medical care, and because this type of vertigo may appear at different times following injury, from 1 day to a few months.
The recent case reports on the causes of secondary BPPV include such as dancing rehearsal [12]. This indicates that even those minor impacts on the head experienced from everyday life to the extent that cannot be defined as trauma, or any physical exercises can cause BPPV. The treatment of minor posttraumatic BPPV is not different from that of BPPV by other causes and its recurrence rate also is known as similar [5]. Therefore, if a BPPV is suspected, the physician must check for a head impact even minor such as yoga practice.
Notes
No potential conflict of interest relevant to this article was reported.