안면침범없이 동측 외전신경과 반대쪽 반신마비로 발현한 교뇌연수이음부 경색
Ponto-medullary Junction Infarction Presenting as Ipsilateral Abducens Nerve Palsy and Contralateral Hemiparesis without Facial Involvement
Article information
Trans Abstract
Raymond syndrome is a pontine syndrome consisting of ipsilateral abducens nerve palsy, contralateral facial paralysis, and contralateral hemiparesis. However, subsequent clinical observations argued on the presentation of facial involvement. The only differentiating point between the facial including called classic type and the facial sparing Raymond syndrome is the location of the lesion. The classic type involves abducens nerve, corticofacial, and corticospinal tracts; while in the facial sparing type, corticofacial tracts, and peripheral facial nerves are spared. We experienced a 78-year-old man presented with sudden onset dizziness, binocular horizontal diplopia, and right-sided motor weakness. Neurological examination showed he had left abducens nerve palsy and right hemiparesis without facial involvement. Brain magnetic resonance imaging showed acute ischemic infarction in the left ponto-medullary junction. Regardless of the presence or absence of facial palsy, the combination of abducence nerve palsy and contralateral hemiparesis should direct the clinician’s attention towards the medial ventral caudal ponto-medullary junction.
INTRODUCTION
Raymond syndrome, named after a French neurologist Fulgence Raymond, consists of ipsilateral abducens nerve palsy, contralateral central type facial paresis, and contralateral hemiparesis [1]. Whether this rarely reported syndrome necessarily includes central facial paralysis is debated [2]. This syndrome should be differentiated from Millar Gubbler syndrome, which involves ipsilateral abducens and facial nerve paralysis and contralateral hemiplegia [3,4]. Raymond syndrome is an extremely rare neurologic entity. Also, although rare in foreign reports, there are cases reported in the form of cases. The authors had experienced a case of ipsilateral abducens nerve palsy and contralateral hemiparesis without facial involvement called Raymond syndrome without facial involvement. Thereby we report this case with a review of the related literatures with informed consent from the patient.
CASE REPORT
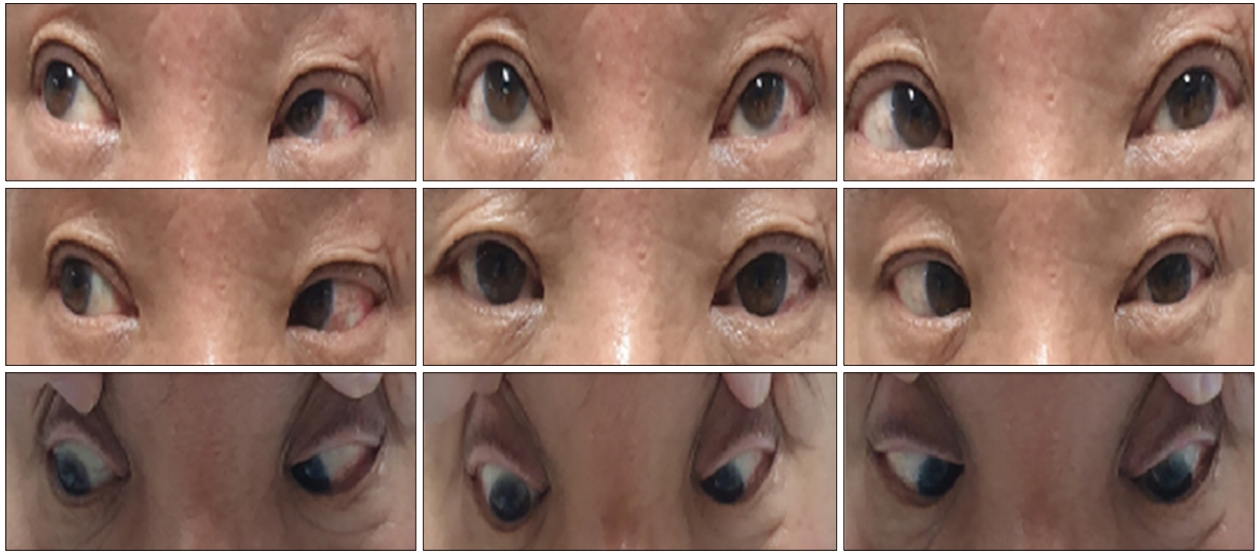
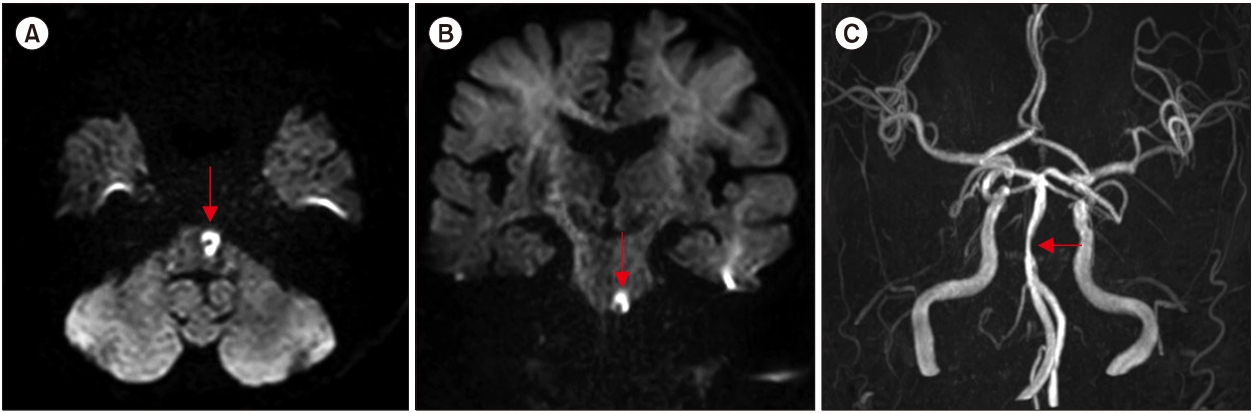
A 78-year-old man presented with binocular horizontal diplopia of sudden onset, worsened by directing gaze to the left, dizziness, and right-sided motor weakness. His past medical history included essential hypertension treated with a calcium channel blocker, a 60-pack-per-year smoking history, and moderate alcohol consumption. Neurological examination showed abduction limitation of the left eye (Fig. 1) and right hemiparesis (arm and leg, grade 3 on the Medical Research Council grading system). Both spontaneous and voluntary facial movements were normal. Pupils were equal, round, and reactive to light and accommodation. He did not exhibit ptosis. Deep tendon reflexes were normal and there was positive Babinski sign on right side. There was no ataxia or sensory deficit. Gait was unremarkable due to weakness. Laboratory examinations were normal except elevated cholesterol level (total cholesterol 224 mg/dL, low density lipid 145 mg/dL). Magnetic resonance imaging (MRI) performed 1 day after the onset of symptoms showed an ischemic lesion in the left antero-medial pontomedullary junction (Fig. 2A, B). Intracranial magnetic resonance angiography evealed mild focal basilar arterial stenosis (Fig. 2C). Dizziness and diplopia resolved partially over several days after clopidogrel and atorvastatin treatment. But the patient was handicapped by the right hemiparesis.
DISCUSSION
The French neurologist Fulgence Raymond described the clinical picture that bears his name in 1895 [1,2]. Raymond hypothesized that a lesion in the lower medial pons damaged the abducens nerve and the nondecussated corticofacial and pyramidal tracts, but spared the more lateral facial nerve. Landry previously reported a similar patient with a hemisensory deficit in addition to hemiplegia [1]. However, after reviewing Raymond’s original description, Wolfe disagreed with the hypothesis, citing the patient’s development of a cerebral right hemiplegia, aphasia, and difficulty recognizing her husband’s face [2], arguing that Raymond’s explanation for the findings was unlikely; thus, not even Raymond’s patient had “Raymond syndrome.” In both Raymond’s and Landry’s patients, the hemiplegia included central facial palsy. The lesion lies in the medial ventral caudal pons. Other eponymous syndromes of the caudal pons include Millard-Gubler syndrome (peripheral facial palsy plus contralateral hemiplegia) and Foville syndrome (peripheral facial palsy and horizontal gaze palsy plus contralateral hemiplegia), both caused by lesions extending more laterally and dorsally [2,5].
A patient with abducens nerve paresis and contralateral hemiparesis sparing the face caused by a lesion in the pontomedullary junction was recently diagnosed with Raymond syndrome [6]. Others suggested using the eponym only when central facial palsy is present [7]. This controversy likely reflects uncertainty about the anatomical course of corticofacial fibers in the brainstem. Innovations in technology have dramatically expanded our knowledge of the functional and neuroanatomical structures. Urban et al. [8] used transcranial magnetic stimulation to study the course of corticofacial projections in the human brainstem in patients with and without central facial paresis due to focal ischemic lesions of the brainstem (Fig. 3). In correlation with brain MRI, they identified corticofacial fibers may loop down into the ventral part of the upper medulla, cross the midline, and ascend in the dorsolateral medullary region to the facial nucleus in some patients. Their findings provide additional evidence suggesting that a contralateral central facial paresis may occur due to a focal lesion at the pontine base [8]. This anatomical variability might reflect the phylogenetically recent appearance of the corticospinal and corticobulbar tracts. Interestingly, the corticofacial projection has also been identified in paramedial lemniscus as an aberrant pyramidal tract in the pons through the upper medulla [9].

Anatomical relationship between the abducens nerve, facial nerve, corticofacial tract, and corticospinal tract (infarcted area is shown in gray).
Abducens nerve palsy should be differentiated from the effects of lesions of the abducens nucleus. The latter contains abducens motor neurons that supply the lateral rectus muscle and abducens internuclear neurons that project, via the medial longitudinal fasciculus, to the medial rectus subdivision of the contralateral oculomotor nucleus. Thus, lesions of the abducens nucleus cause an ipsilateral, conjugate gaze palsy with defective abduction in the ipsilateral eye and defective adduction in the contralateral eye [10,11]. Abducens nucleus lesions are often accompanied by deficits due to the involvement of adjacent structures in the pons. Thus, an ipsilateral, peripheral facial nerve palsy is a common but not invariable accompaniment because of the proximity of the fascicles of this nerve to the abducens nucleus [12].
Alternatively, a very small ponto-medullary junction lesion may only partially damage the corticospinal tracts. Regardless of the presence or absence of central facial palsy, the combination of abducens nerve palsy and contralateral hemiparesis should direct the clinician’s attention towards the medial ventral caudal pons.
Notes
No potential conflict of interest relevant to this article was reported.
Acknowledgements
This paper was supported by the Wonkwang University in 2019.