양성돌발두위현훈이 있는 골다공증 노인 환자에서 졸레드론산 주사의 효과
Intravenous Zoledronic Acid in Elderly Patients with Benign Paroxysmal Positional Vertigo and Osteoporosis
Article information
Trans Abstract
Objectives:
Benign paroxysmal positional vertigo (BPPV), a common cause of vertigo in the elderly, shares common pathogenic mechanisms with osteoporosis. We investigated the efficacy and safety of intravenous zoledronic acid in elderly patients with BPPV and osteoporosis.
Methods:
We performed a 3-year observational study with elderly patients who were diagnosed with BPPV and osteoporosis. The recurrence of BPPV and changes in bone mineral densitometry (BMD) scores were evaluated one year after the administration of intravenous zoledronic acid.
Results:
We enrolled 101 elderly patients with BPPV and 54 of them (53.5%) met the diagnostic criteria for osteoporosis. Intravenous zoledronic acid was administered in 51 patients. The recurrence of BPPV was observed in only two of 49 patients (4.1%) at 1 year’s follow-up. The mean lowest T-score of BMD improved from –3.23±0.51 to –3.05±0.58 (p=0.001).
Conclusions:
Our study showed that the treatment of osteoporosis can be considered to prevent the recurrence of BPPV in the elderly. Further placebo-controlled studies are needed to estimate accurately the efficacy of zoledronic acid in the prevention of recurrence of BPPV in the elderly.
INTRODUCTION
Dizziness and vertigo are common neurological symptoms and they are responsible for approximately 3.5% of the patients visits the emergency room [1]. Most patients with vertigo have benign diseases of the ear, including benign paroxysmal positional vertigo (BPPV), vestibular neuritis, and Menière’s disease, but it can be a presentation of severe central nervous system diseases, such as cerebrovascular diseases, vestibular migraine, and epilepsy [2].
BPPV is more prevalent in the elderly. One population-based study showed that the 1-year prevalence of BPPV rose from 0.5% in people aged 18 to 39 years to 3.4% in those aged 60 years and older, and the cumulative incidence of BPPV reached almost 10% by the age of 80 years [3]. Although the high incidence of BPPV in the elderly may be related to the high comorbidity of secondary causes of BPPV, such as head trauma, Menière’s diseases, and diabetes mellitus [4], it is also possible that the high prevalence of osteoporosis in the elderly may affect the increased risk of BPPV, because the suggested pathogenesis of BPPV, age-related weakening of otoconia in the semicircular canal of the inner ear, shares common mechanisms of impaired calcium metabolism and decreased blood levels of vitamin D with osteoporosis [5]. One recent study using national database also showed that osteoporosis increased the risk of BPPV in the population aged 50 years and older [6].
Zoledronic acid is an intravenous bisphosphonate drug used for the treatment of osteoporosis. It has a prolonged dosing interval with a once-yearly infusion, which can be an advantage over other bisphosphonates in the aspect of drug adherence because it is estimated that less than 40% of patients who are prescribed oral bisphosphonates are still taking them after 1 year [7,8].
In the present study, we hypothesized that intravenous zoledronic acid therapy could reduce the recurrence of BPPV in the elderly, and investigated the efficacy and safety of intravenous zoledronic acid in elderly patients with BPPV and osteoporosis.
MATERIALS AND METHODS
We designed a single-center, 3-year observational study from January 2017 to December 2019. This study protocol was approved by Institutional Review Board of Konkuk University Hospital (No. KUH1170165) and informed consents were obtained from all included patients.
From January 2017 to December 2018, we prospectively investigated consecutive patients with BPPV who were 65 years of age or over at their visit to the emergency room or outpatient clinic of Konkuk University Medical Center in Seoul, Korea. The diagnosis of BPPV was based on the history and observing positional nystagmus during specific provocative maneuvers. Clinical symptom of BPPV was characterized by brief vertigo, usually lasting than 1 minute induced by a change in head position with respect to gravity [9]. We excluded patients when they were under treatment for osteoporosis or had causes of secondary BPPV, such as acute traumatic brain injury, recent head surgery, vestibular neuritis, or current inner ear infection. Patients with a previous history of BPPV were not excluded, but its association with osteoporosis was estimated (Fig. 1).
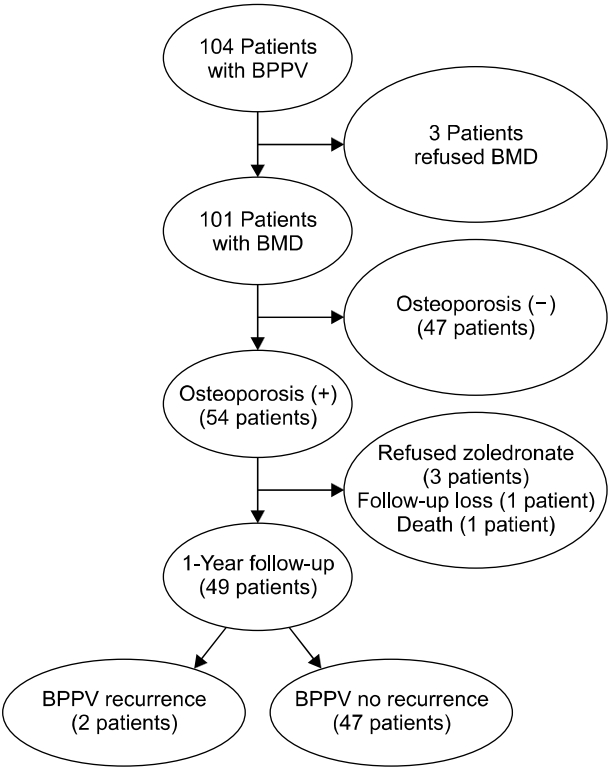
Schematic diagram of the numbers of patients with benign paroxysmal positional vertigo (BPPV), bone mineral densitometry (BMD) studies, zoledronic acid treatment, and the recurrence of BPPV.
After the diagnosis of BPPV, patients underwent bone mineral densitometry (BMD) at the lumbar vertebrae and bilateral femur neck. The lowest T-score less than –2.5 was regarded as osteoporosis. Intravenous zoledronic acid was administered in patients who were diagnosed with osteoporosis, and the development of adverse effects from zoledronic acid therapy was monitored during the 3 days. The recurrence of BPPV was evaluated 1 year after zoledronic acid therapy during an outpatient clinic visit or by telephone interview and follow-up BMD studies were performed in patients who visited the outpatient clinic. The recurrence of BPPV was confirmed by the presence of typical history and observing positional nystagmus during specific provocative maneuvers.
We studied the difference in the clinical features between the patients with and without osteoporosis using Student t-test and chi-squared tests. Paired t-tests were used to compare the initial and follow-up BMD T-scores. The level of significance was set at a p-value of <0.05.
RESULTS
A total of 104 patients aged 65 years and over were treated for BPPV during the 2-year inclusion period. A previous history of BPPV was documented in 14 patients. Noncontrast brain computed tomography was performed in 92 patients (88.5%) who visited emergency room for BPPV and diffusion-weighted magnetic resonance imaging was performed to rule out the possible vascular or other organic causes of vertigo in 68 patients (65.4%). Three patients were excluded from the study because they refused to perform BMD during the acute period of BPPV. The mean lowest T-score of 101 patients who underwent BMD was –2.44±1.11 (range, –4.90 to 1.00). More than half of the patients (54 of 101, 53.5%) were diagnosed as osteoporosis. Osteoporosis was more common in females and advanced ages, but there was no difference in the previous history of BPPV between the two groups (Table 1). Intravenous zoledronic acid was administered in 51 patients (51 of 54, 94.4%) excluding three patients who refused to be treated with zoledronic acid, and eight of them (8 of 51, 15.7%) complained of treatment-related adverse effects (flu-like symptoms). The adverse effects were mild in most patients and easily treated with acetaminophen or nonsteroid anti-inflammatory drugs. However, one patient revisited the emergency room 1 day after zoledronic acid infusion for fever and severe myalgia.
The recurrence of BPPV was followed up in 49 patients by outpatient clinic visits (30 patients) or telephone calls (19 patients) 1 year later, excluding two patients (one was lost to follow-up and the other had a sudden death). BPPV recurrence was observed in only two patients (2/49, 4.1%). Follow-up BMD studies were performed in 23 patients and the mean lowest T-score improved from –3.23±0.51 to –3.05±0.58 (p=0.001). Fracture did not occur during the follow-up period after the treatment of zoledronic acid.
DISCUSSION
We showed that osteoporosis was common in elderly patients with BPPV. After treatment with intravenous zoledronic acid, approximately 15% of the patients (8 of 51, 15.7%) experienced flu-like adverse events, and only two of 49 patients (4.1%) experienced a recurrence of BPPV during the 1-year follow-up.
Most patients with BPPV are idiopathic in nature, but many medical conditions may predispose an individual to development of idiopathic BPPV. BPPV is associated with diabetes mellitus, chronic thyroiditis, hyperlipidemia, stroke, osteoporosis, and decreased blood level of vitamin D [10,11]. In particular, there are several well-designed reports on the association of BPPV with osteoporosis and decreased blood level of vitamin D, and the high recurrence of the BPPV can be in part explained by osteoporosis and the decreased blood level of vitamin D [5,12].
BPPV is usually a self-limited condition and its treatment includes canalith repositioning maneuvers and vestibular rehabilitation. Medical therapy is not recommended as a primary treatment for BPPV [9]. However, previous studies showed that the recurrence of BPPV was quite common with a recurrence rate of 10% to 43%, and most recurrences occurred within 2 years after the initial event [12]. The high recurrence rate may be related to the predisposing conditions of BPPV, such as impaired calcium metabolism or low vitamin D levels, which were not corrected after the diagnosis of BPPV, because low blood levels of vitamin D and osteoporosis have been frequently reported in association with BPPV [13].
Zoledronic acid increases bone mineral density and reduces the risk of subsequent fractures. It is recommended both for moderate and high-risk osteoporosis groups [14]. Although there is no direct evidence that zoledronic acid can increase the stability of the otoconia of the inner ear, zoledronic acid may reduce the risk of BPPV, considering that osteoporosis and BPPV share some common pathogenetic mechanisms. With its drug adherence advantage, zoledronic acid has been tried for patients with several neurological diseases, such as stroke and Alzheimer’s dementia [15,16]. The occurrence of flu-like symptoms is one of the most troublesome adverse effects of zoledronic acid in the elderly, and the incidence of this adverse effect was not different from that of patients with osteoporosis in previous studies [14].
This study had several limitations. We performed a single-center study and could include only a limited number of patients. Therefore, it is difficult to apply our results to the general population and further studies with long-term follow-ups are necessary to confirm the efficacy and safety of zoledronic acid in elderly patients with BPPV. The lack of analysis of other important clinical factors for osteoporosis, such as vitamin D blood levels was also another limitation. Most importantly, we did not perform a placebo-controlled study and the information on the recurrence of BPPV was obtained by telephone interviews with some patients. Because we included elderly patients with a high possibility of recall bias, we admit that the effect of zoledronic acid in the prevention of BPPV may be overestimated. Additional prospective placebo-controlled study with a long follow-up period should be performed to clearly demonstrate the efficacy of zoledronic acid in the prevention of recurrence of BPPV in the elderly. However, we think our study has clinical implications in that it suggests that osteoporosis treatment for elderly patients with BPPV may be useful in preventing the recurrence of the troublesome disease.
Notes
This study was supported by the Daewoong Pharmaceutical Company. No other potential conflict of interest relevant to this article was reported.

