Articles
- Page Path
- HOME > Res Vestib Sci > Volume 23(1); 2024 > Article
-
Case Report
- A case of cerebellopontine angle meningioma presenting as neurovascular compression syndrome of the 8th cranial nerve
-
Jeongin Jang1
 , Sung Kwang Hong1,2
, Sung Kwang Hong1,2 , Joonho Song3
, Joonho Song3 , Hyung-Jong Kim1
, Hyung-Jong Kim1 , Hyo-Jeong Lee1,2
, Hyo-Jeong Lee1,2
-
Clinical and Experimental Otorhinolaryngology 2024;23(1):28-31.
DOI: https://doi.org/10.21790/rvs.2023.141
Published online: March 15, 2024
1Department of Otorhinolaryngology-Head and Neck Surgery, Hallym University College of Medicine, Chuncheon, Korea
2Laboratory of Brain & Cognitive Sciences for Convergence Medicine, Hallym University College of Medicine, Chuncheon, Korea
3Department of Neurosurgery, Hallym University College of Medicine, Chuncheon, Korea
- Corresponding Author: Hyo-Jeong Lee Department of Otolaryngology, Hallym University Medical Center, 22 Gwanpyeong-ro 170beon-gil, Dongan-gu, Anyang, 14068, Korea E-mail: hyojlee@hallym.ac.kr
© 2024 The Korean Balance Society
This is an open access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 227 Views
- 2 Download
Abstract
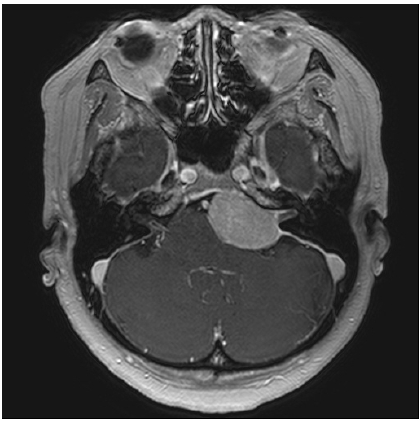
- A 54-year-old female patient presented with paroxysmal tinnitus and vertigo for 2 years, which have repeatedly occurred while rotating her neck, and lasted about 10 seconds. An anticonvulsant medication was prescribed with a diagnosis of microvascular compression syndrome on the 8th cranial nerve and audiovestibular evaluation and magnetic resonance imaging (MRI) scan were appointed a week later. In her next visit, she reported the disappearance of paroxysmal audiovestibular symptoms after medication. In the left ear, canal paresis and abnormal auditory brainstem response were observed. In MRI, a large meningioma in the cerebellopontine angle in the vicinity of the internal auditory canal orifice was detected, that was surgically resected by a neurosurgeon. After surgical removal of the tumor, she reported continuous dizziness due to vestibular nerve injury, but the paroxysmal attack of tinnitus and vertigo disappeared without anticonvulsant medication. This case suggests that an imaging study is mandatory when diagnosing microvascular compression syndrome on the 8th cranial nerve.
INTRODUCTION
CASE REPORT
DISCUSSION
-
Funding/Support
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean Government (2022R1A2C1004862).
-
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
-
Availability of Data and Materials
All data generated or analyzed during this study are included in this published article. For other data, these may be requested through the corresponding author.
-
Authors' Contributions
Conceptualization, Resources: HJL, JS; Data curation: JJ; Formal analysis: JJ, SKH; Funding acquisition, Project administration, Supervision, Validation: HJL; Investigation: SKH; Methodology: HJL, HJK; Writing–original draft: HJL, JJ; Writing–review & editing: all authors.
All authors read and approved the final manuscript.
ARTICLE INFORMATION


- 1. Hüfner K, Barresi D, Glaser M, et al. Vestibular paroxysmia: diagnostic features and medical treatment. Neurology 2008;71:1006–1014.ArticlePubMed
- 2. Strupp M, Lopez-Escamez JA, Kim JS, et al. Vestibular paroxysmia: diagnostic criteria. J Vestib Res 2016;26:409–415.ArticlePubMedPMC
- 3. Jannetta PJ, Møller MB, Møller AR. Disabling positional vertigo. N Engl J Med 1984;310:1700–1705.ArticlePubMed
- 4. Koo YJ, Kim HJ, Choi JY, Kim JS. Vestibular paroxysmia associated with typewriter tinnitus: a case report and literature review. J Neurol 2021;268:2267–2272.ArticlePubMedPDF
- 5. Levine RA. Typewriter tinnitus: a carbamazepine-responsive syndrome related to auditory nerve vascular compression. ORL J Otorhinolaryngol Relat Spec 2006;68:43–47.ArticlePubMedPDF
- 6. De Ridder D, Vanneste S, Adriaensens I, Lee AP, van de Heyning P, Möller A. Vascular compression of the cochlear nerve and tinnitus: a pathophysiological investigation. Acta Neurochir (Wien) 2012;154:807–813.ArticlePubMedPDF
- 7. De Ridder D, Heijneman K, Haarman B, van der Loo E. Tinnitus in vascular conflict of the eighth cranial nerve: a surgical pathophysiological approach to ABR changes. Prog Brain Res 2007;166:401–411.PubMed
- 8. Shandal V, Fernández-Conejero I, Sekula R, Crammond D, Thirumala P, Anetakis K, et al. Microvascular decompression for cranial nerve disorders. In: Seubert CN, Balzer JR, editors. Koht, Sloan, Toleikis’s monitoring the nervous system for anesthesiologists and other health care professionals. 3rd ed. Springer, Cham; 2022. p. 465-493.
REFERENCES
Figure & Data
References
Citations


 KBS
KBS
 PubReader
PubReader ePub Link
ePub Link Cite
Cite