Articles
- Page Path
- HOME > Res Vestib Sci > Volume 23(1); 2024 > Article
-
Review Article
- Virtual reality simulators for temporal bone dissection: overcoming limitations of previous models
-
Temuulen Batsaikhan1,2
 , Young Joon Seo1,2
, Young Joon Seo1,2
-
Clinical and Experimental Otorhinolaryngology 2024;23(1):1-10.
DOI: https://doi.org/10.21790/rvs.2024.002
Published online: March 15, 2024
1Department of Otorhinolaryngology, Yonsei University Wonju College of Medicine, Wonju, Korea
2Research Institute of Hearing Enhancement, Yonsei University Wonju College of Medicine, Wonju, Korea
- Corresponding Author: Young Joon Seo Department of Otorhinolaryngology, Yonsei University Wonju College of Medicine, 20 Ilsan-ro, Wonju 26426, Korea E-mail: okas2000@yonsei.ac.kr
© 2024 The Korean Balance Society
This is an open access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 755 Views
- 11 Download
Abstract
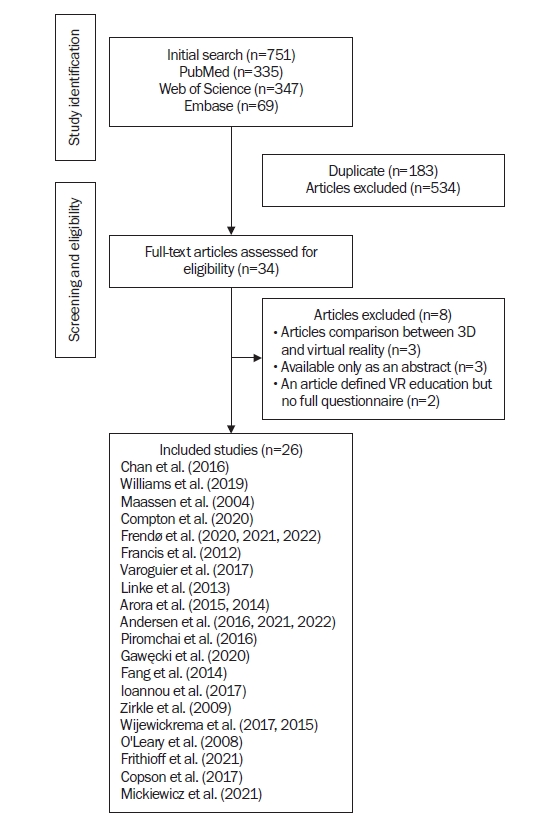
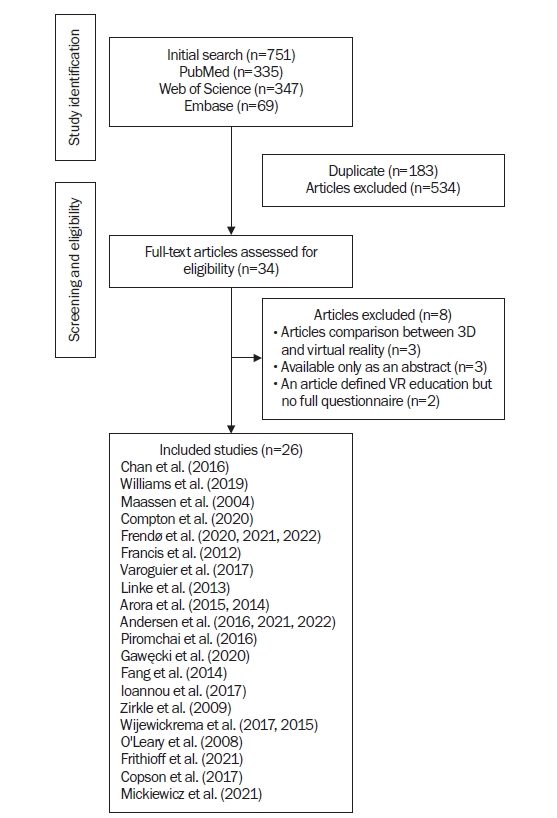
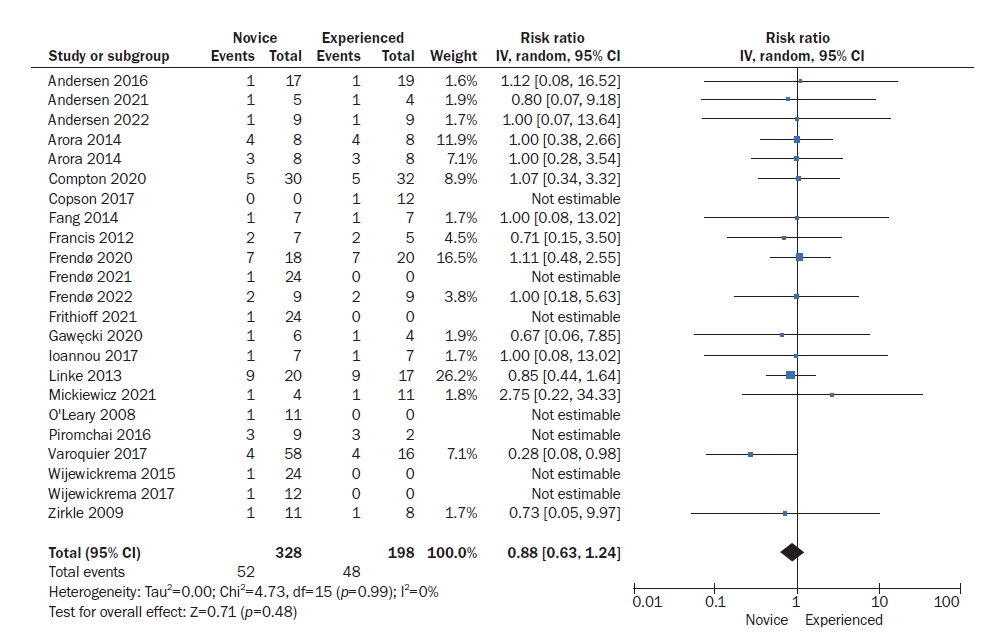
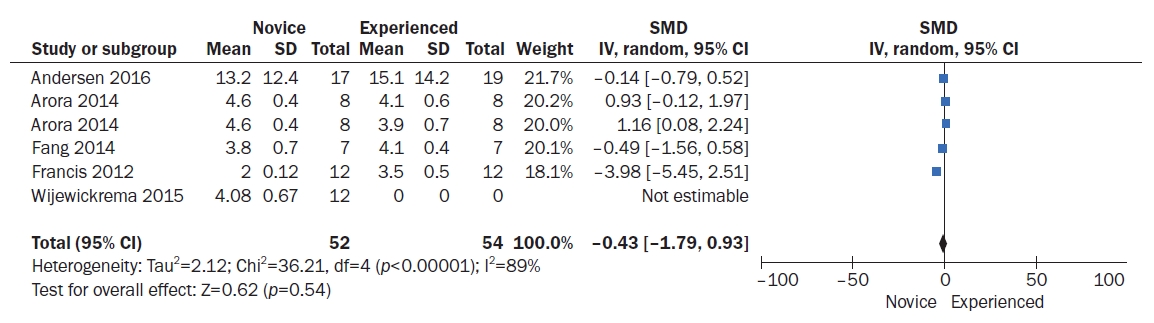
- Temporal bone dissection is a critical skill for otolaryngology trainees: however, it is challenging to master due to the complex anatomy and limited exposure to cadaveric specimens. The aim of this review was to develop and evaluate a novel virtual reality (VR) simulator for temporal bone dissection, addressing the limitations of previous simulators reported in the literature. A comprehensive literature search was conducted in the PubMed, Embase, and Cochrane Library databases from inception to September 2022. The search was limited to studies that evaluated the effectiveness of VR simulators for temporal bone dissection. The quality of the included studies was assessed using the Cochrane Risk of Bias Tool. The results showed that VR simulators can significantly improve temporal bone dissection skills, including anatomical knowledge, instrument handling, and surgical performance. Compared to traditional training methods, VR simulation was associated with faster learning curves, better retention of skills, and greater confidence among trainees. However, some limitations of current VR models were identified, including the lack of haptic feedback, limited realism, and short duration of practice. VR simulators are a valuable adjunct to traditional methods for temporal bone dissection training. The recently developed VR simulator addressed the limitations of previous simulators and demonstrated its potential to enhance the training of clinicians in temporal bone dissection. Future directions for research include further validation of the simulator and exploration of its potential for use in clinical settings.
INTRODUCTION
METHODS
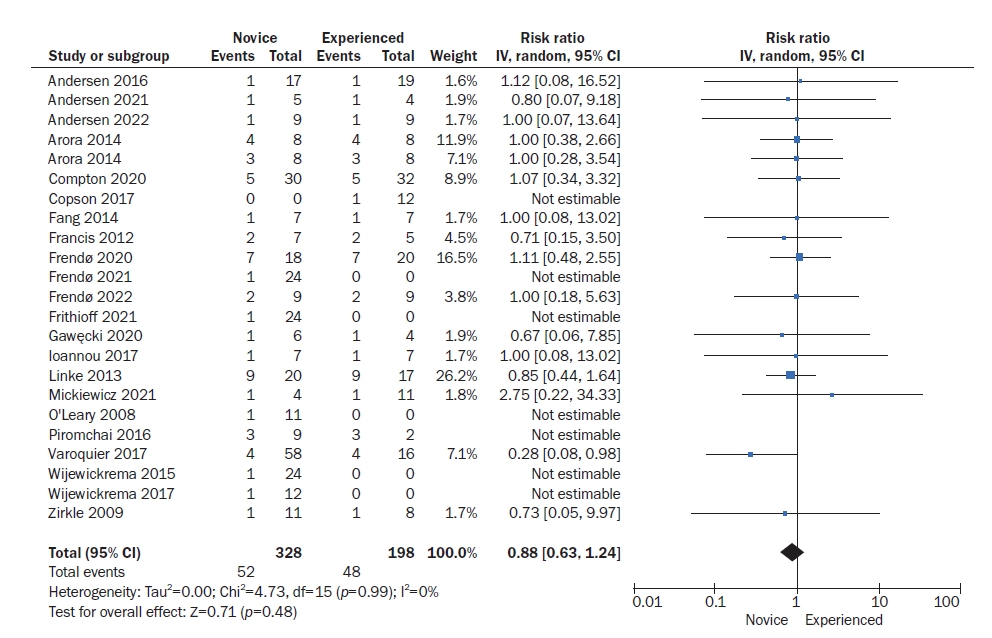
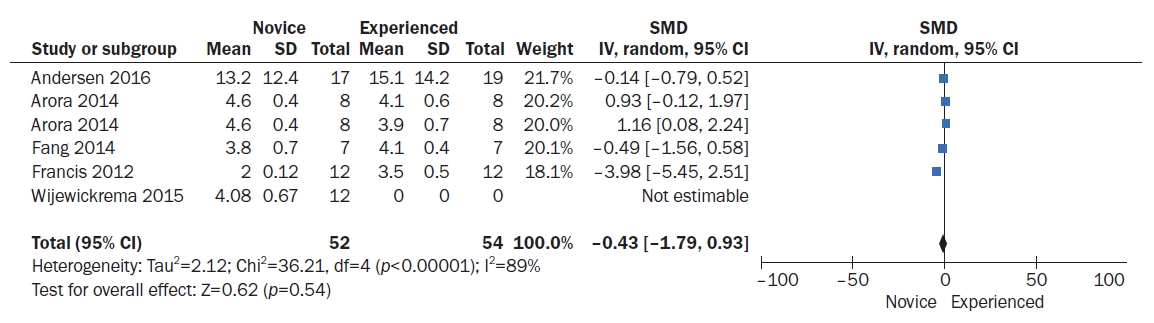
RESULTS
DISCUSSION
-
Funding/Support
This research was supported by “Regional Innovation Strategy (RIS)” through the National Research Foundation of Korea(NRF) funded by the Ministry of Education (MOE) (2022RIS-005) and by Korean Fund for Regenerative Medicine funded by Ministry of Science and ICT, and Ministry of Health and Welfare (21C0721L1, Republic of Korea).
-
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
-
Availability of Data and Materials
All data generated or analyzed during this study are included in this published article. For other data, these may be requested through the corresponding author.
-
Authors' Contributions
Conceptualization, Project administration, Validation, Visualization: TB, YJS; Data curation, Formal analysis, Investigation, Methodology, Resources, Software: TB; Funding acquisition: YJS; Writing–original draft: TB, YJS; Writing–review & editing: TB, YJS.
All authors read and approved the final manuscript.
ARTICLE INFORMATION
| Title | Developers | Developed year | Developed platform | Purpose | Outcomes | Limitation | Image database | Data acquisition |
|---|---|---|---|---|---|---|---|---|
| VR temporal bone surgery simulator | Arora et al. [4] | 2014 | VoxelMan | Case-specific surgical rehearsal in VR temporal bone surgery | Improved surgical skills, planning, training, and confidence | Limited sample size | CT image | Likert scale |
| VR temporal bone surgery simulator | Arora et al. [5] | 2015 | Unity | Teaching temporal bone dissection | Improved surgical skill training and surgical anatomy | Limited number of participants | CT image | Likert scale |
| VR temporal bone IHD implantation simulator | Maassen et al. [6] | 2004 | REALAX | Temporal bone IHD implantation in a VR environment | No significant difference between VR and surgical implantation | A limited number of participants | Cadaver and patient’s CT | Qualitative measurement |
| VR temporal bone surgery simulator | Francis et al. [7] | 2012 | VoxelMan | Teaching temporal bone surgery | Improved objective structured assessment of technical skills | Limited number participants | CT image | Likert scale |
| No direct comparison with other training methods | ||||||||
| VR temporal bone surgery simulator | Fang et al. [8] | 2014 | Visible Ear Simulator | Teaching temporal bone dissection | Improved surgical skills and confidence | Limited number of participants | CT image | Likert scale |
| VR temporal bone surgery simulator | Chan et al. [9] | 2016 | CardinalSim | To create a preoperative VR environment that allows increasing practical temporal bone-related surgery | The same anatomical or pathological features were observed in both intraoperative video and simulation | No objective measurement of performance improvement | Patient’s temporal bone CT and MRI | Qualitative measurement |
| VR temporal bone surgery simulator | Linke et al. [10] | 2013 | VoxelMan | Teaching temporal bone surgery | More experienced surgeons fewer injuries with better score | No direct comparison with other training methods | CT image | Modified final product analysis scale |
| VR temporal bone dissection simulator | Varoquier et al. [11] | 2017 | VoxelMan | Teaching temporal bone dissection | Experienced surgeons better overall scores and faster than novices | No direct comparison with other training methods | CT image | Likert scale |
| VR temporal bone dissection simulator | Frendø et al. [12] | 2020 | NVIDIA Omniverse | Decentralized temporal bone VR surgery training | Improved performance in temporal bone dissection tasks | No direct comparison with other training methods | CT image | Welling scale |
| VR temporal bone dissection simulator | Zirkle et al. [13] | 2009 | VoxelMan | Teaching temporal bone dissection | Experienced trainees had better outcome than novice | No direct comparison with other training methods | CT image | Quantitative measurement |
| VR temporal bone surgery simulator | Gawęcki et al. [14] | 2020 | NVIDIA | Teaching antromastoidectomy surgery | Improved surgical skills after repeated training | Limited number of participants | CT image | Likert scale |
| Limited sample size | ||||||||
| VR temporal bone dissection simulation | Andersen et al. [15] | 2022 | NVIDIA Geforce | Self-assessment VR simulation mastoidectomy effects during cadaveric dissection | Improved dissection performance during VR simulation with higher performance during cadaveric dissection | Cohort reference as a historic controls | CT image | Welling scale |
| VR temporal bone mastoidectomy simulation | Andersen et al. [16] | 2016 | Visible Ear Simulator | Training mastoidectomy VR training | Final performance had increased after VR training | No direct comparison with other training methods | CT image | Welling scale |
| VR temporal bone simulation | Mickiewicz et al. [17] | 2021 | (Geomagic touch haptic device) | Teaching antromastoidectomy surgery | Improved surgical performance | Limited number of participants | CT image | Likert scale |
| VR temporal bone surgery simulation | Copson et al. [18] | 2017 | (VR temporal bone simulator) | Teaching cochlear implant surgery | Improved cochlear implant surgery performance after VR simulation | Limited number of participants | Cadaver’s temporal bone | Global competency scale |
| VR temporal bone surgery simulation | Frithioff et al. [19] | 2021 | Visible Ear Simulator | Teaching cochlear implantation | There are no differences between conventional and screen-based VR simulation | Limited number of participants | CT image | Qualitative measurement |
| Medical students | ||||||||
| VR temporal bone mastoidectomy surgery simulator | Frendø et al. [20] | 2021 | Visible Ear Stimulator | Teaching cochlear implant surgery | Improved surgical skills and confidence | Limited sample size | CT image | Cochlear implant surgery assessment tool |
| VR temporal bone surgery simulator | Frendø et al. [21] | 2022 | Visible Ear Simulator | Cochlear implantation on VR simulation | Improved surgical skills and confidence | No direct comparison with other training methods | CT image | Likert scale |
| VR temporal bone surgery simulator | Williams et al. [22] | 2019 | NVIDIA Omniverse | Teaching temporal bone surgery | Positive feedback from trainees | No direct comparison with another training method | Cadaver’s temporal bone CT | Likert scale |
| Medical students | ||||||||
| VR temporal bone surgery simulator | Compton et al. [23] | 2020 | NVIDIA Omniverse | Temporal bone surgery training | Positive feedback from participants | No direct comparison with another training method | Cadaver’s temporal bone CT form DICOM files | Likert scale |
| VR temporal bone surgery simulator | Andersen et al. [24] | 2021 | NVIDIA | Teaching mastoidectomy | Usefulness for presurgical planning | Limited number of participants | Clinical CBCT image | Likert scale |
| VR temporal bone surgery simulator | Piromchai et al. [25] | 2016 | NVIDIA 3D | Anatomical variation in VR cochlear implant surgery | Improved performance in temporal bone dissection tasks | Limited number of participants | CT image | Global rating scale |
| VR temporal bone surgery simulator | Ioannou et al. [26] | 2017 | Visible Ear Simulator | Difference between experts’ and trainees’ surgical performance | Experts spend less time and shorter drilling paths than trainees | Limited number of participants | CT image | Quantitative measurement |
| VR temporal bone dissection simulation | Wijewickrema et al. [27] | 2017 | NA | Training temporal bone cochlear implant surgery | Positive feedback from participants | Limited number of participants | Cadaver’s CT image | Likert scale |
| VR temporal bone surgery simulation | O’Leary et al. [28] | 2008 | CSIRO | Teaching temporal bone surgery | Improved surgical ability, planning, and technique of temporal bone surgery | Limited number of participants | CT image | Temporal bone assessment criteria |
| VR temporal bone surgery simulation | Wijewickrema et al. [29] | 2015 | (VR temporal bone simulator) | Teaching temporal bone surgery | Improved surgical skills after VR training and positive feedback from participants | No direct comparison with other training methods | CT image | Quantitative measurement |
| Medical students |
- 1. Rose AS, Kimbell JS, Webster CE, Harrysson OL, Formeister EJ, Buchman CA. Multi-material 3D models for temporal bone surgical simulation. Ann Otol Rhinol Laryngol 2015;124:528–536.ArticlePubMedPDF
- 2. Sieber D, Erfurt P, John S, et al. The OpenEar library of 3D models of the human temporal bone based on computed tomography and micro-slicing. Sci Data 2019;6:180297. ArticlePubMedPMCPDF
- 3. Longfield EA, Brickman TM, Jeyakumar A. 3D printed pediatric temporal bone: a novel training model. Otol Neurotol 2015;36:793–795.PubMed
- 4. Arora A, Swords C, Khemani S, et al. Virtual reality case-specific rehearsal in temporal bone surgery: a preliminary evaluation. Int J Surg 2014;12:141–145.ArticlePubMed
- 5. Arora A, Hall A, Kotecha J, et al. Virtual reality simulation training in temporal bone surgery. Clin Otolaryngol 2015;40:153–159.ArticlePubMed
- 6. Maassen MM, Schwaderer E, Heinrich B, Herberhold S, Mauz PS, Dammann F. Comparison of the implantability of electronic hearing devices in a virtual reality planning environment and in human temporal bones. Acta Otolaryngol 2004;124:1039–1045.ArticlePubMed
- 7. Francis HW, Malik MU, Diaz Voss Varela DA, et al. Technical skills improve after practice on virtual-reality temporal bone simulator. Laryngoscope 2012;122:1385–1391.ArticlePubMedPDF
- 8. Fang TY, Wang PC, Liu CH, Su MC, Yeh SC. Evaluation of a haptics-based virtual reality temporal bone simulator for anatomy and surgery training. Comput Methods Programs Biomed 2014;113:674–681.ArticlePubMed
- 9. Chan S, Li P, Locketz G, Salisbury K, Blevins NH. High-fidelity haptic and visual rendering for patient-specific simulation of temporal bone surgery. Comput Assist Surg (Abingdon) 2016;21:85–101.ArticlePubMedPDF
- 10. Linke R, Leichtle A, Sheikh F, et al. Assessment of skills using a virtual reality temporal bone surgery simulator. Acta Otorhinolaryngol Ital 2013;33:273–281.PubMedPMC
- 11. Varoquier M, Hoffmann CP, Perrenot C, Tran N, Parietti-Winkler C. Construct, face, and content validation on Voxel-Man® simulator for otologic surgical training. Int J Otolaryngol 2017;2017:2707690. ArticlePubMedPMCPDF
- 12. Frendø M, Konge L, Cayé-Thomasen P, Sørensen MS, Andersen SA. Decentralized virtual reality training of mastoidectomy improves cadaver dissection performance: a prospective, controlled cohort study. Otol Neurotol 2020;41:476–481.ArticlePubMed
- 13. Zirkle M, Roberson DW, Leuwer R, Dubrowski A. Using a virtual reality temporal bone simulator to assess otolaryngology trainees. Laryngoscope 2007;117:258–263.ArticlePubMed
- 14. Gawęcki W, Węgrzyniak M, Mickiewicz P, Gawłowska MB, Talar M, Wierzbicka M. The impact of virtual reality training on the quality of real antromastoidectomy performance. J Clin Med 2020;9:3197. ArticlePubMedPMC
- 15. Andersen SA, Frithioff A, von Buchwald JH, Sørensen MS, Frendø M. Am I doing this right?: structured self-assessment during simulation training of mastoidectomy improves cadaver dissection performance: a prospective educational study. Eur Arch Otorhinolaryngol 2023;280:97–103.ArticlePubMedPDF
- 16. Andersen SA, Konge L, Cayé-Thomasen P, Sørensen MS. Retention of mastoidectomy skills after virtual reality simulation training. JAMA Otolaryngol Head Neck Surg 2016;142:635–640.ArticlePubMed
- 17. Mickiewicz P, Gawęcki W, Gawłowska MB, Talar M, Węgrzyniak M, Wierzbicka M. The assessment of virtual reality training in antromastoidectomy simulation. Virtual Real 2021;25:1113–1121.ArticlePDF
- 18. Copson B, Wijewickrema S, Zhou Y, et al. Supporting skill acquisition in cochlear implant surgery through virtual reality simulation. Cochlear Implants Int 2017;18:89–96.ArticlePubMed
- 19. Frithioff A, Frendø M, Mikkelsen PT, Sørensen MS, Andersen SA. Cochlear implantation: exploring the effects of 3D stereovision in a digital microscope for virtual reality simulation training: a randomized controlled trial. Cochlear Implants Int 2022;23:80–86.ArticlePubMed
- 20. Frendø M, Frithioff A, Konge L, Sørensen MS, Andersen SA. Cochlear implant surgery: learning curve in virtual reality simulation training and transfer of skills to a 3D-printed temporal bone: a prospective trial. Cochlear Implants Int 2021;22:330–337.ArticlePubMed
- 21. Frendø M, Frithioff A, Konge L, Cayé-Thomasen P, Sørensen MS, Wuyts Andersen SA. Cochlear implant surgery: virtual reality simulation training and transfer of skills to cadaver dissection-a randomized, controlled trial. J Int Adv Otol 2022;18:219–224.PubMedPMC
- 22. Williams C, Wijewickrema S, Piromchai P, O’Leary S. The effect of practice distribution on skill retention in virtual reality temporal bone surgery training. In: 2019 IEEE 32nd International Symposium on Computer-Based Medical Systems (CBMS). Cordoba, Spain; 2019. p. 495-500.
- 23. Compton EC, Agrawal SK, Ladak HM, et al. Assessment of a virtual reality temporal bone surgical simulator: a national face and content validity study. J Otolaryngol Head Neck Surg 2020;49:17. ArticlePubMedPMCPDF
- 24. Andersen SA, Varadarajan VV, Moberly AC, Hittle B, Powell KA, Wiet GJ. Patient-specific virtual temporal bone simulation based on clinical cone-beam computed tomography. Laryngoscope 2021;131:1855–1862.ArticlePubMedPDF
- 25. Piromchai P, Ioannou I, Wijewickrema S, et al. Effects of anatomical variation on trainee performance in a virtual reality temporal bone surgery simulator. J Laryngol Otol 2017;131(S1):S29–S35.Article
- 26. Ioannou I, Zhou Y, Wijewickrema S, et al. Comparison of experts and residents performing a complex procedure in a temporal bone surgery simulator. Otol Neurotol 2017;38:e85–e91.ArticlePubMed
- 27. Wijewickrema S, Copson B, Zhou Y, et al. Design and evaluation of a virtual reality simulation module for training advanced temporal bone surgery. In: 2017 IEEE 30th International Symposium on Computer-Based Medical Systems (CBMS). Thessaloniki, Greece; 2017. p. 7-12.
- 28. O’Leary SJ, Hutchins MA, Stevenson DR, et al. Validation of a networked virtual reality simulation of temporal bone surgery. Laryngoscope 2008;118:1040–1046.ArticlePubMed
- 29. Wijewickrema S, Piromchai P, Zhou Y, et al. Developing effective automated feedback in temporal bone surgery simulation. Otolaryngol Head Neck Surg 2015;152:1082–1088.ArticlePubMedPDF
- 30. Timonen T, Dietz A, Linder P, et al. The effect of virtual reality on temporal bone anatomy evaluation and performance. Eur Arch Otorhinolaryngol 2022;279:4303–4312.ArticlePubMedPMCPDF
- 31. Lee C, Wong GK. Virtual reality and augmented reality in the management of intracranial tumors: a review. J Clin Neurosci 2019;62:14–20.ArticlePubMed
- 32. Timonen T, Iso-Mustajärvi M, Linder P, et al. Virtual reality improves the accuracy of simulated preoperative planning in temporal bones: a feasibility and validation study. Eur Arch Otorhinolaryngol 2021;278:2795–2806.ArticlePubMedPMCPDF
- 33. Reddy-Kolanu G, Alderson D. Evaluating the effectiveness of the Voxel-Man TempoSurg virtual reality simulator in facilitating learning mastoid surgery. Ann R Coll Surg Engl 2011;93:205–208.ArticlePubMedPMC
REFERENCES
Figure & Data
References
Citations


 KBS
KBS
 PubReader
PubReader ePub Link
ePub Link Cite
Cite