Abstract
-
Objectives
- Pulse wave velocity (PWV) is a known indicator of arterial stiffness reflecting vascular damage. However, there are few reports of the relationship between PWV and dizziness/vertigo of a vascular origin. We investigated whether the PWV value could be useful as an ancillary measurement for identifying the etiology of dizziness/vertigo.
-
Methods
- We enrolled dizzy patients from March 2016 to December 2018. The patients with posterior circulation stroke presenting with dizziness/vertigo were categorized as having central vertigo. The patients with vertigo due to benign paroxysmal positional vertigo, Ménière disease, or acute unilateral vestibulopathy were categorized as having peripheral vertigo. The PWV value, ankle-brachial index (ABI), and traditional vascular risk factors were collected.
-
Results
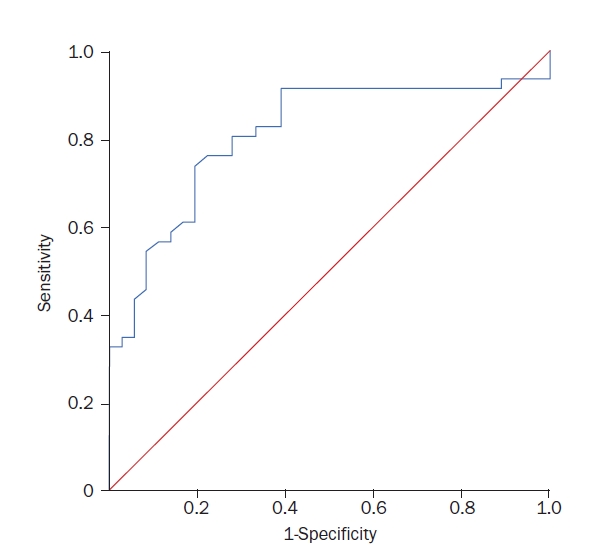
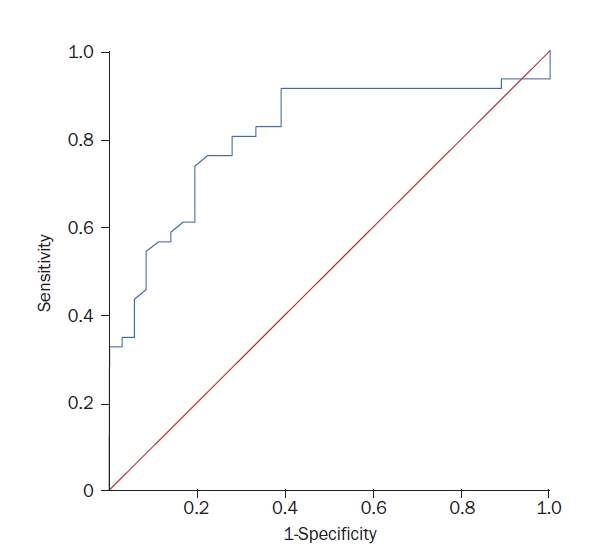
- We consecutively enrolled a total of 93 participants. The PWV values were higher in the central vertigo group (p<0.001), but ABI did not differ between the groups. Among the vascular risk factors, the number of patients with diabetes mellitus, dyslipidemia, and male patients was significantly higher in the central vertigo group. The brachial-ankle PWV (baPWV) values were higher in the central vertigo group, even after adjusting for confounding factors (p<0.01). The receiver operating characteristic curve showed that the sensitivity was 74% and specificity was 81% when the mean baPWV value was 14.78 m/sec.
-
Conclusions
- Increased baPWV values were observed in patients with dizziness/vertigo due to stroke. Measurement of the baPWV value could be an ancillary test for evaluating the cause of dizziness/vertigo, even though more convincing evidence is still required.
-
Keywords: Pulse wave analysis; Dizziness; Vertigo; Ischemic stroke
INTRODUCTION
Dizziness is one of the most commonly reported major medical symptoms in general medical clinics, accounting for approximately 3% to 5% of visits across various care settings [1]. In clinical practice, dizziness presents with a range of etiologies, making the diagnosis of dizzy patients challenging, especially when their symptoms and signs are vague or equivocal [2]. Considering that about 10% of dizzy patients have a central brainstem lesion, particularly those with acute vestibular syndrome (AVS), evaluating the central causes of dizziness/vertigo becomes essential. Recent case series-based studies have underscored this necessity by revealing that vertigo may manifest as a primary or sole symptom of stroke [3-6].
In cases of AVS, stroke is assessed through a combination of bedside neurotological examination, such as the head impulse-nystagmus-test of skew (HINTS) battery, along with brain imaging, including the blood vessels [7,8]. In episodic vestibular syndrome (EVS), vascular causes, including transient ischemic attacks, are considered for patients with vascular risk factors and transient neurological deficits. However, diagnosing EVS resulting from vascular causes is more challenging, as the diagnosis often relies on patient history rather than neurotological examination, mainly due to the fact that most patients usually present to hospitals during interictal periods, when they do not exhibit any symptoms or signs [7].
Arterial stiffness increases with age and has been suggested as a surrogate marker for atherosclerosis and an independent cardiovascular risk factor [9-11]. Measurement of the carotid-femoral pulse wave velocity (cfPWV) is considered the gold standard method for assessing central artery stiffness [12]. Elevated cfPWV is associated with traditional risk factors such as hypertension, diabetes mellitus, inflammatory conditions, and disease of the coronary, peripheral, cerebral arteries, and aorta. However, cfPWV has a limited use for general practitioners, because this parameter is usually hard to obtain. An easier alternative is the measurement of brachial-ankle PWV (baPWV), which has become available as a means of measuring PWV [13]. baPWV is widely used in clinical practice because baPWV measurement provides automated results and is more convenient than cfPWV measurement. The value of baPWV has been shown to be reproducible and well correlated with that of cfPWV [13].
In a clinical setting, the diagnostic work-up of dizziness/vertigo becomes complex when brain imaging is unavailable. Neurotological examinations, including the HINTS battery, may be challenging for general physicians and primary care doctors to perform effectively. If there were a simple and easily applicable laboratory or imaging tool to aid in diagnosing vascular vertigo, it would undoubtedly benefit general practitioners. Furthermore, there are limited reports on the relationship between baPWV and dizziness/vertigo. Thus, our study investigated the baPWV value across several subtypes of dizziness/vertigo and aimed to determine whether baPWV values can predict cases of stroke presenting with dizziness/vertigo.
METHODS
This study was approved by the Institutional Review Board of Chonnam National University Hospital (CRE 16106-7). All subjects provided written informed consent in accordance with the Declaration of Helsinki.
Study Population
We prospectively enrolled patients with dizziness/vertigo who visited Chonnam National University Hospital from March 2016 to December 2018. Patients were included as follows: (1) they had suffered acute prolonged dizziness/vertigo for 24 hours or more due to ischemic stroke in posterior circulation, which was categorized as central vertigo; or (2) they complained of dizziness/vertigo due to acute unilateral vestibulopathy (AUVP)/vestibular neuritis, benign paroxysmal positional vertigo (BPPV), or Ménière’s disease (MD), which was categorized as peripheral vertigo. Each case of peripheral vertigo was diagnosed based on recently proposed diagnostic criteria (Supplementary Table 1) [14-17].
Brain Magnetic Resonance Imaging
The diagnosis of all patients with central vertigo was confirmed using brain magnetic resonance imaging (MRI). According to the imaging protocol of the hospital, the patients who were suspected of having acute stroke underwent MRI in the emergency department immediately after admission to the hospital. The MRI protocol consisted of T2- and T1-weighted imaging, diffusion-weighted imaging, fluid-attenuated inversion recovery imaging, gradient echo imaging, and time-of-flight magnetic resonance angiography (MRA) in sequence. Relevant arterial steno-occlusion was defined as symptomatic arterial steno-occlusion with moderate to severe stenosis (≥50% of luminal narrowing) or occlusion based on MRA results.
Measurement of Brachial-ankle Pulse Wave Velocity, Blood Pressure, and Ankle-brachial Index
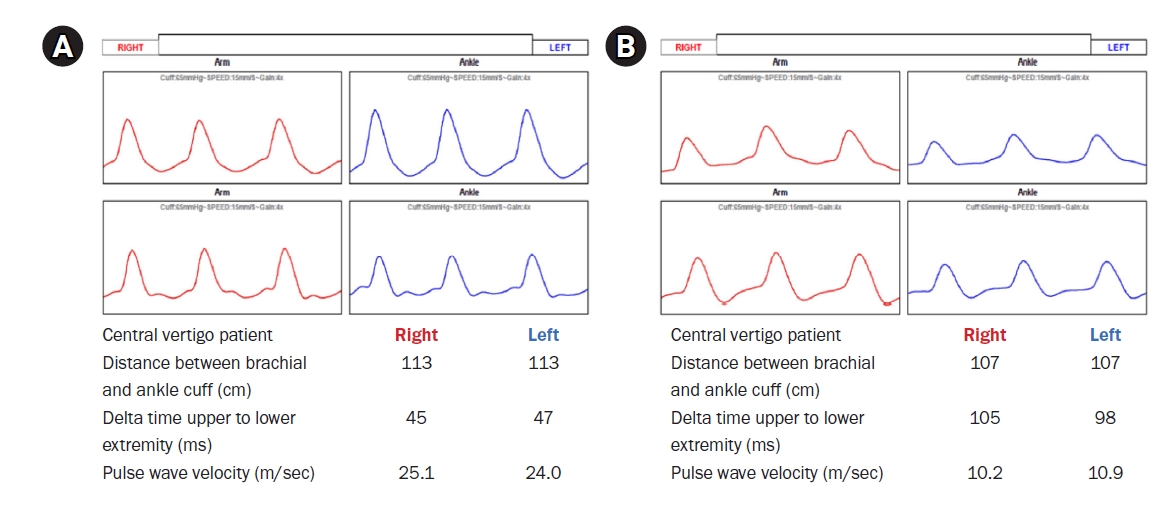
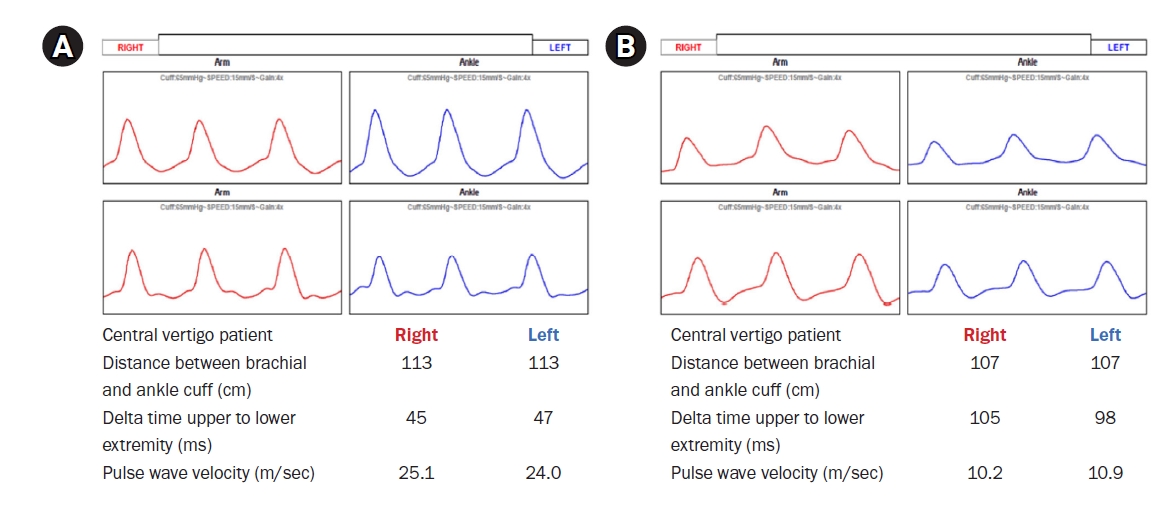
The baPWV and ankle-brachial index (ABI) were obtained through a single measurement with the patient in the supine position using an automated device (ANGIOLAB 4; Spead-Doppler-Systeme Vertriebs GmbH), which has been previously validated [12]. This device simultaneously measures arterial pulse waves and systolic/diastolic arterial pressures in both the brachial and posterior tibial arteries using the oscillometric method. The transmission time for travel between the right arm and both ankles was calculated using the waveform. The transmission distance between the right brachium and ankle was automatically calculated based on the patient’s height. The baPWV on each side was determined by dividing the transmission distance by the transmission time. In the analyses, we utilized the higher values of baPWV (normal range, lower than 15.50 m/sec) and brachial blood pressures (including systolic, diastolic, and mean arterial pressure) on both sides. Patients with a baPWV value greater than 15.50 m/sec were categorized into the higher baPWV group. Mean arterial pressure was calculated by adding the systolic pressure to twice the diastolic pressure and dividing the total by three. The ABI was calculated as the lower measurement of systolic pressure in the legs divided by the higher measurement of systolic pressure in the arms (Fig. 1). ABI values were categorized as follows: ABI <0.5, severe peripheral arterial occlusive disease (PAOD); 0.5<ABI<0.9, mild to moderate PAOD; 0.9<ABI<1.3, normal; and ABI >1.3, noncompressible (medial sclerosis, calcification). We excluded patients with a low ABI value indicative of PAOD (<0.9), as PAOD can affect the baPWV value and thereby compromise the reliability of arterial stiffness detection [12]. The baPWV and ABI measurements were conducted during the symptomatic period, mostly within 1 to 3 days following the onset of symptoms, in central vertigo and AUVP, both of which are included within the category of AVS. Conversely, these tests were performed during the interictal period in patients with BPPV and MD (EVS).
Clinical Variables and Risk Factors
We collected the baseline characteristics including age, sex, and traditional vascular risk factors, such as hypertension, diabetes mellitus, current smoking (defined as cigarette smoking within the last 5 years), dyslipidemia, atrial fibrillation, and previous stroke (both ischemic and hemorrhagic).
Statistical Analysis
Subjects were divided into two groups: central vertigo due to posterior circulation stroke and peripheral vertigo due to AUVP, BPPV, or MD. Data are presented as mean±standard deviation for continuous variables or frequencies for categorical variables. The chi-square test and Fisher exact test were used to compare categorical variables, while the Mann-Whitney U-test and the Kruskal-Wallis test were employed to assess continuous variables in univariate analyses. Multivariable logistic regression analysis was used to evaluate whether the baPWV value might be an independent predictor of central vertigo. Odds ratios and 95% confidence intervals were calculated. A p-value of <0.05 was considered statistically significant. IBM SPSS Statistics for Windows (ver. 21.0, IBM Corp.) was used for all statistical analyses.
RESULTS
Baseline Characteristics
A total of 93 participants were enrolled in this study, with a mean age of 63.9±12.8 years. Among them, 45 patients were classified into the peripheral vertigo group, which included individuals with AUVP (n=17), BPPV (n=21), and MD (n=7). The central vertigo group comprised 48 patients, consisting of 21 with anterior inferior cerebellar artery (AICA) territory infarction, 11 with posterior inferior cerebellar artery (PICA) territory infarction, and 16 with superior cerebellar artery (SCA) territory infarction. The clinical characteristics of the subjects are summarized in Table 1.
Comparisons of the Two Groups: Central Vertigo vs. Peripheral Vertigo
In this study, male patients were more prevalent in the central vertigo group. Additionally, the baPWV values were significantly higher in the central vertigo group (p<0.001 for right, left, and mean baPWV), while the ABI values did not display any significant difference. In terms of vascular risk factors, diabetes mellitus and dyslipidemia were notably more frequent in the central vertigo group. However, no significant differences were observed in terms of atrial fibrillation and history of previous stroke between the two groups (Table 1).
Significance of Brachial-ankle Pulse Wave Velocity Values
Even after adjusting for confounding variables (Table 2), the baPWV value remained higher in the central vertigo group. Categorizing the participants into higher and lower baPWV groups based on a cut-off value of 15.50 m/sec, independent clinical predictors for central vertigo were identified, with male sex showing statistical significance (p=0.003, Table 3). The associations between baPWV values and central vertigo were also confirmed in the multivariate logistic regression analysis (Table 3). The receiver operating characteristic curve demonstrated a sensitivity of 74% and specificity of 81% when the mean baPWV value was 14.78 m/sec (Fig. 2).
Subgroup Analysis within Both Peripheral and Central Vertigo Groups
To investigate potential differences between subtypes within each group, we compared the PWV parameters and clinical factors. Within the peripheral vertigo group, we compared the three subtypes (AUVP, BPPV, MD), but no significant differences were found in demographic findings, PWV values, or vascular risk factors among the three subgroups (Supplementary Table 2). Similarly, within the central vertigo group, no differences were observed between the three subtypes (AICA, PICA, SCA) (Supplementary Table 3).
DISCUSSION
Our study demonstrates that baPWV values were higher in patients with acute vascular vertigo/dizziness due to cerebellar infarction, compared to those in patients with peripheral vertigo. A mean baPWV value of 14.78 m/sec exhibited a sensitivity of 74% and specificity of 81% when distinguishing between central and peripheral vertigo.
Stroke can manifest as acute prolonged dizziness/vertigo, and these symptoms may be the sole manifestation of stroke [18]. As vascular vertigo mostly presents as acute or transient episodes, and only rarely as positional vestibular syndrome [19], the diagnosis of stroke in patients with dizziness/vertigo can be challenging. Approximately 20% of ischemic strokes occur in the territory of the posterior (vertebrobasilar) circulation, and dizziness/vertigo is the most common symptom of vertebrobasilar ischemia. Although isolated dizziness/vertigo is uncommon in central lesions, including strokes, inferior cerebellar and small brainstem infarctions have been increasingly recognized as a cause of isolated vertigo due to advancements in clinical neurotology and neuroimaging. Differentiating isolated vertigo of vascular origin from more benign inner ear disorders is important, given the differences in management and prognosis. Misdiagnosing acute stroke can lead to significant morbidity and mortality. Thus, distinguishing isolated vertigo caused by vascular causes from benign inner ear disorders is crucial [20]. Bedside neurologic examination, including the HINTS battery, is a sensitive and essential approach for identifying stroke in patients presenting with acute dizziness/vertigo [8]. However, emergency physicians, who lack specialization in neurotology, might encounter challenges in administering the HINTS test or interpreting its results [21]. While brain MRI is more accurate, its availability is limited in most emergency departments, and even MRI could lead to false-negative results in the first 24 hours after a posterior circulation stroke [7]. Recently, certain laboratory tests, such as assessing an increased neutrophil-to-lymphocyte ratio and elevated neuron-specific enolase levels, or neuro-sonological tests, such as vertebral artery extracranial color-coded duplex sonography, have been utilized in diagnosing patients with acute dizziness/vertigo to distinguish between stroke origin and other peripheral causes. Our study also offers evidence for an easy and simple screening tool for predicting stroke among patients with acute dizziness/vertigo [22,23].
Arterial stiffness is recognized as an independent predictor of cardiovascular disease, including stroke, in healthy subjects [24]. It aids in assessing the condition of the vasculature [24]. The measurement of PWV is employed for this purpose, and it is derived by calculating the transmission time between pulse pressure waves at two sites, such as the carotid-radial, carotid-femoral, or brachial-ankle PWV. Elevated arterial stiffness can lead to abnormal vascular flow and unusual pulsation, causing disruptions in vascular endothelial function, even in the microvasculature [12,25]. Additionally, the decreased vascular reactivity caused by microvascular damage can result in microvascular ischemia [26]. A recent systematic review suggested an association between elevated PWV and cerebral microvascular ischemia [12].
In this study, we observed elevated baPWV in vertigo cases caused by stroke. Prior evidence has suggested that arterial stiffness may influence the cerebral microvasculature, rendering affected individuals more susceptible to stroke [10,12]. In a previous study using transcranial Doppler, an increased pulsatility index could reflect microvasculature abnormality in cerebral vessels [27]. Similarly, the elevated baPWV, which measures arterial stiffness, and microvasculature abnormalities might reflect vascular function within the brain. Our findings suggest that baPWV could serve as a surrogate marker for stroke development in patients with isolated dizziness and/or vertigo; however, further studies are warranted.
A low ABI implies peripheral arterial stenosis. Several studies have indicated that baPWV’s diagnostic and risk-predictive value is not high in patients with peripheral artery disease [12]. In such cases, baPWV does not have significant clinical importance, and using it as a clinical indicator is not recommended [12]. As a result, we excluded patients with an ABI value of less than 0.9.
The pathomechanism of AUVP, one of the most common causes of peripheral vertigo, remains controversial. While AUVP is typically associated with inflammatory diseases of the inner ear, such as viral infections, vascular risk factors, including arterial stiffness, might contribute to the development of AUVP in line with the vascular theory [28]. However, our study did not reveal differences in the baPWV value among peripheral vertigo subgroups. This result may support the inflammation theory of AUVP, but this will also need further examination in future studies with a larger sample size.
Traditional stroke risk factors such as old age, hypertension, diabetes mellitus, hyperlipidemia, and smoking play a pivotal role in the diagnosis of central vertigo. Subgroup analysis within both central and peripheral vertigo groups did not reveal any differences in stroke risk factors, as expected. In our study, the prevalence of atrial fibrillation had a borderline statistically significant difference between the central and peripheral groups. Symptoms and signs of central vertigo were relatively mild in our study population, irrespective of the presence of stroke. In general, cardioembolic stroke may cause severe dysfunction. Consequently, our patients, who presented with isolated dizziness/vertigo, likely had a lower prevalence of cardioembolism. Conversely, mild strokes in the posterior circulation, as observed in our patients, often involve large artery disease or small vessel occlusion [29]. Additionally, the relatively small sample size in our study may have impacted the prevalence of atrial fibrillation. The central vertigo group had a higher number of male patients, possibly reflecting the higher prevalence of stroke among males [29]. Conversely, peripheral vertigo, particularly BPPV, is more common among women, according to previous studies [30]. This could account for the observed gender imbalance in our study.
There are some limitations to this study. Firstly, it is important to note that this is a single-referral center study with a relatively small sample size, which might have led to reduced statistical power. Secondly, we did not conduct an analysis of the subtypes of ischemic stroke in this research. Stroke can develop from various etiologies, including large artery atherosclerosis and cardiogenic embolism. It is possible that PWV values could vary based on the subtypes of ischemic stroke. Thirdly, rather than directly measuring blood flow in major blood vessels like transcranial Doppler, PWV measures systemic arterial stiffness, so it may not accurately reflect selective arterial stiffness in the posterior circulation. These aspects may warrant further investigation in future studies.
In conclusion, the baPWV value may be used as a predictor of central vertigo even though more convincing evidence is required. Future research should provide more robust evidence for the role of arterial stiffness in central vertigo.
ARTICLE INFORMATION
-
Funding/Support
None.
-
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
-
Availability of Data and Materials
All data generated or analyzed during this study are included in this published article. For other data, these may be requested through the corresponding author.
-
Authors' Contributions
Conceptualization: BHC, JMK, SHL; Formal analysis: BHC, JMK; Investigation: YIK; Writing–original draft: BHC, JMK; Writing–review & editing: YIK, SHL.
All authors read and approved the final manuscript.
SUPPLEMENTARY MATERIALS
Supplementary materials can be found via https://doi.org/10.21790/rvs.2024.003/
Supplementary Table 1.
Diagnostic criteria of acute unilateral vestibulopathy/vestibular neuritis, benign paroxysmal positional vertigo, and Ménière’s disease
rvs-2024-003-Supplementary-Table-1.pdf
Fig. 1.Examples of brachial-ankle pulse wave velocity (baPWV) in central vertigo (A) and peripheral vertigo (B). (A) The baPWV result of a 67-year-old man who was diagnosed with central vertigo (superior cerebellar arterial territory infarction). The baPWV is 25.1 m/sec on the right and 24.0 m/sec on the left. (B) The baPWV results of a 58-year-old woman who was diagnosed with peripheral vertigo (benign paroxysmal positional vertigo). The baPWV is 10.2 m/sec on the right and 10.9 m/sec on the left.
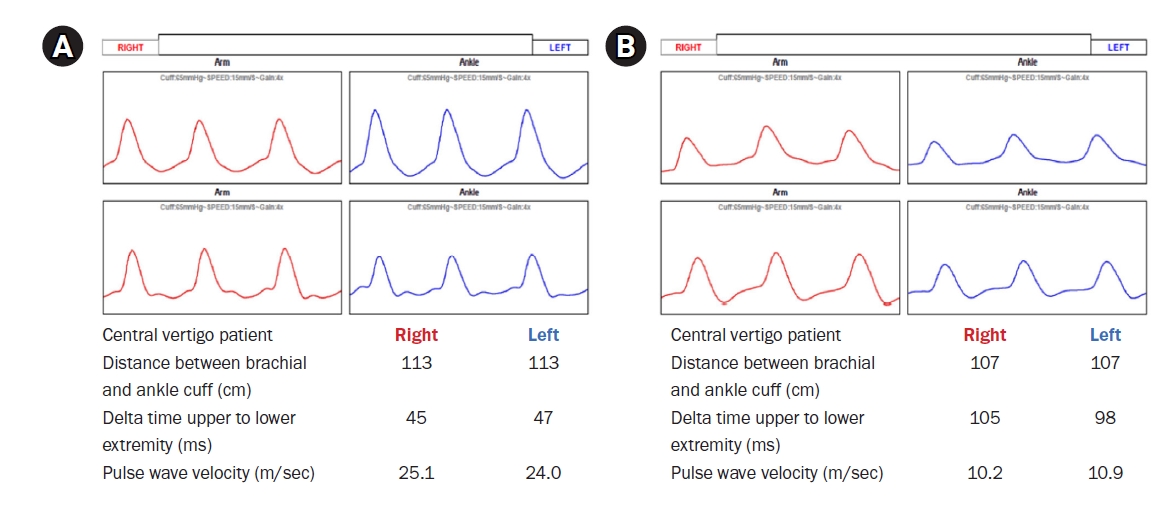
Fig. 2.The receiver operating characteristic curve for differentiating peripheral vertigo from central vertigo (sensitivity, 74% and specificity, 81% at mean pulse wave velocity value of 14.78 m/sec).
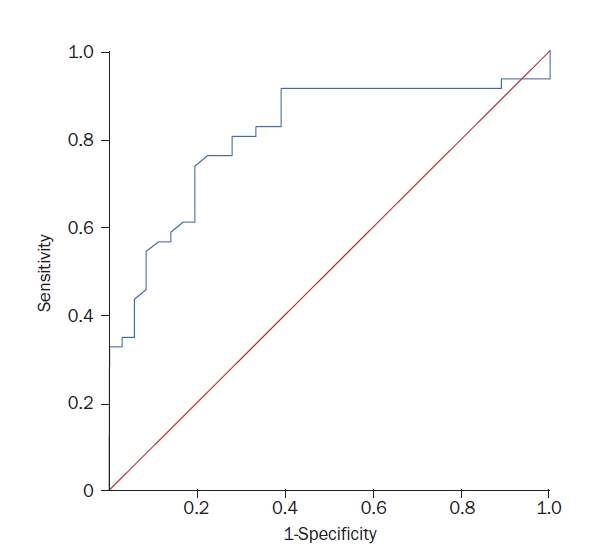
Table 1.Demographic and clinical characteristics of the study population
|
Characteristic |
Peripheral vertigo |
Central vertigo |
p-value |
|
No. of patients |
45 |
48 |
|
|
Age (yr) |
64.18±13.18 |
63.60±12.57 |
0.830 |
|
Male sex |
19 (42.2) |
31 (64.6) |
0.031 |
|
Hypertension |
17 (37.8) |
26 (54.2) |
0.113 |
|
Diabetes mellitus |
6 (13.3) |
17 (35.4) |
0.014 |
|
Atrial fibrillation |
4 (8.9) |
7 (14.6) |
0.417 |
|
Previous stroke |
1 (2.2) |
5 (10.4) |
0.205 |
|
Dyslipidemia |
10 (22.2) |
23 (47.9) |
0.006 |
|
Smoking |
7 (15.6) |
18 (37.5) |
0.075 |
|
baPWV |
|
|
|
|
Right |
12.20±2.80 |
17.37±4.88 |
<0.001 |
|
Left |
12.66±3.44 |
18.67±5.77 |
<0.001 |
|
Mean |
12.43±2.99 |
18.67±5.77 |
<0.001 |
|
Ankle-brachial index |
|
|
|
|
Right |
1.17±0.12 |
1.13±0.14 |
0.180 |
|
Left |
1.15±0.10 |
1.14±0.10 |
0.500 |
|
Mean |
1.16±0.10 |
1.13±0.10 |
0.210 |
Table 2.The right baPWV values after adjusting for significant vascular risk factors
|
baPWV (m/sec) |
Peripheral vertigo (n=45) |
Central vertigo (n=48) |
Adjusted p-value |
|
Right |
12.20±2.80 |
17.37±4.88 |
<0.001 |
|
Left |
12.66±3.44 |
18.67±5.77 |
<0.001 |
|
Mean |
12.43±2.99 |
18.67±5.77 |
<0.001 |
Table 3.Independent predictors of central vertigo
|
Predictor |
Univariate analysis
|
Multivariate analysis
|
|
OR (95% CI) |
p-value |
Adjusted OR (95% CI) |
p-value |
|
Age |
1.00 (0.97–1.03) |
0.830 |
|
|
|
Male sex |
2.50 (1.08–5.76) |
0.032 |
13.08 (2.37–72.07) |
0.003 |
|
Hypertension |
1.95 (0.85–4.46) |
0.120 |
|
|
|
Diabetes mellitus |
3.57 (1.26–10.12) |
0.017 |
4.75 (0.53–42.36) |
0.160 |
|
Atrial fibrillation |
1.71 (0.46–6.29) |
0.420 |
|
|
|
Dyslipidemia |
3.50 (1.41–8.70) |
0.007 |
1.23 (0.26–5.86) |
0.800 |
|
Smoking |
2.48 (0.90–6.86) |
0.080 |
|
|
|
Pulse wave velocity |
|
|
|
|
|
Right |
1.50 (1.23–1.83) |
<0.001 |
1.58 (1.24–2.02) |
<0.001 |
|
Left |
1.37 (1.18–1.60) |
<0.001 |
1.39 (1.18–1.64) |
<0.001 |
|
Mean |
1.33 (1.15–1.53) |
<0.001 |
1.37 (1.17–1.60) |
<0.001 |
REFERENCES
- 1. Newman-Toker DE, Hsieh YH, Camargo CA, Pelletier AJ, Butchy GT, Edlow JA. Spectrum of dizziness visits to US emergency departments: cross-sectional analysis from a nationally representative sample. Mayo Clin Proc 2008;83:765–775.ArticlePubMedPMC
- 2. Kroenke K, Lucas CA, Rosenberg ML, et al. Causes of persistent dizziness. A prospective study of 100 patients in ambulatory care. Ann Intern Med 1992;117:898–904.ArticlePubMed
- 3. Lee H, Kim HJ, Koo JW, Kim JS. Superior divisional vestibular paresis in anterior inferior cerebellar artery infarction. J Neurol Sci 2009;285:250–253.ArticlePubMed
- 4. Lee H. Neuro-otological aspects of cerebellar stroke syndrome. J Clin Neurol 2009;5:65–73.PubMedPMC
- 5. Kim JS, Lee H. Inner ear dysfunction due to vertebrobasilar ischemic stroke. Semin Neurol 2009;29:534–540.ArticlePubMedPMC
- 6. Lee H, Kim JS, Chung EJ, et al. Infarction in the territory of anterior inferior cerebellar artery: spectrum of audiovestibular loss. Stroke 2009;40:3745–3751.ArticlePubMed
- 7. Newman-Toker DE, Edlow JA. TiTrATE: a novel, evidence-based approach to diagnosing acute dizziness and vertigo. Neurol Clin 2015;33:577–599.PubMed
- 8. Kattah JC, Talkad AV, Wang DZ, Hsieh YH, Newman-Toker DE. HINTS to diagnose stroke in the acute vestibular syndrome: three-step bedside oculomotor examination more sensitive than early MRI diffusion-weighted imaging. Stroke 2009;40:3504–3510.ArticlePubMedPMC
- 9. Boutouyrie P, Tropeano AI, Asmar R, et al. Aortic stiffness is an independent predictor of primary coronary events in hypertensive patients: a longitudinal study. Hypertension 2002;39:10–15.ArticlePubMedPMCPDF
- 10. Vlachopoulos C, Aznaouridis K, Stefanadis C. Prediction of cardiovascular events and all-cause mortality with arterial stiffness: a systematic review and meta-analysis. J Am Coll Cardiol 2010;55:1318–1327.ArticlePubMed
- 11. Coutinho T, Turner ST, Kullo IJ. Aortic pulse wave velocity is associated with measures of subclinical target organ damage. JACC Cardiovasc Imaging 2011;4:754–761.ArticlePubMed
- 12. Munakata M. Brachial-ankle pulse wave velocity: background, method, and clinical evidence. Pulse (Basel) 2016;3:195–204.ArticlePubMed
- 13. Tanaka H, Munakata M, Kawano Y, et al. Comparison between carotid-femoral and brachial-ankle pulse wave velocity as measures of arterial stiffness. J Hypertens 2009;27:2022–2027.ArticlePubMed
- 14. von Brevern M, Bertholon P, Brandt T, et al. Benign paroxysmal positional vertigo: diagnostic criteria. J Vestib Res 2015;25:105–117.ArticlePubMed
- 15. Lopez-Escamez JA, Carey J, Chung WH, et al. Diagnostic criteria for Menière's disease. J Vestib Res 2015;25:1–7.ArticlePubMedPMC
- 16. Jeong SH, Kim HJ, Kim JS. Vestibular neuritis. Semin Neurol 2013;33:185–194.ArticlePubMed
- 17. Strupp M, Bisdorff A, Furman J, et al. Acute unilateral vestibulopathy/vestibular neuritis: diagnostic criteria. J Vestib Res 2022;32:389–406.ArticlePubMedPMC
- 18. Kim JS, Newman-Toker DE, Kerber KA, et al. Vascular vertigo and dizziness: diagnostic criteria. J Vestib Res 2022;32:205–222.ArticlePubMed
- 19. Lee SH, Kim JS. Acute diagnosis and management of stroke presenting dizziness or vertigo. Neurol Clin 2015;33:687–698.ArticlePubMed
- 20. Choi KD, Lee H, Kim JS. Vertigo in brainstem and cerebellar strokes. Curr Opin Neurol 2013;26:90–95.ArticlePubMedPDF
- 21. Dmitriew C, Regis A, Bodunde O, et al. Diagnostic accuracy of the HINTS exam in an emergency department: a retrospective chart review. Acad Emerg Med 2021;28:387–393.ArticlePubMed
- 22. Lee SH, Yun SJ, Ryu S, et al. Utility of neutrophil-to-lymphocyte ratio (NLR) as a predictor of acute infarction in new-onset acute vertigo patients without neurologic and computed tomography abnormalities. J Emerg Med 2018;54:607–614.ArticlePubMedPMCPDF
- 23. Zuo L, Zhan Y, Liu F, et al. Clinical and laboratory factors related to acute isolated vertigo or dizziness and cerebral infarction. Brain Behav 2018;8:e01092. ArticlePubMed
- 24. Mattace-Raso FU, van der Cammen TJ, Hofman A, et al. Arterial stiffness and risk of coronary heart disease and stroke: the Rotterdam Study. Circulation 2006;113:657–663.ArticlePubMed
- 25. Kinjo Y, Ishida A, Kinjo K, Ohya Y. A high normal ankle-brachial index combined with a high pulse wave velocity is associated with cerebral microbleeds. J Hypertens 2016;34:1586–1593.ArticlePubMed
- 26. Kim YB, Park KY, Chung PW, Kim JM, Moon HS, Youn YC. Brachial-ankle pulse wave velocity is associated with both acute and chronic cerebral small vessel disease. Atherosclerosis 2016;245:54–59.ArticlePubMed
- 27. Ghorbani A, Ahmadi MJ, Shemshaki H. The value of transcranial Doppler derived pulsatility index for diagnosing cerebral small-vessel disease. Adv Biomed Res 2015;4:54. ArticlePubMedPMC
- 28. Ahn SH, Shin JE, Kim CH. Final diagnosis of patients with clinically suspected vestibular neuritis showing normal caloric response. J Clin Neurosci 2017;41:107–110.ArticlePubMed
- 29. Kim JT, Park MS, Choi KH, et al. Clinical outcomes of posterior versus anterior circulation infarction with low national institutes of health stroke scale scores. Stroke 2017;48:55–62.ArticlePubMed
- 30. Bisdorff A, Bosser G, Gueguen R, Perrin P. The epidemiology of vertigo, dizziness, and unsteadiness and its links to co-morbidities. Front Neurol 2013;4:29. ArticlePubMedPMC
Citations
Citations to this article as recorded by

 , Jae-Myung Kim2
, Jae-Myung Kim2 , Young-In Kim3, Seung-Han Lee2
, Young-In Kim3, Seung-Han Lee2


 KBS
KBS
 PubReader
PubReader ePub Link
ePub Link Cite
Cite