Abstract
-
Objectives
- The aim of the study was to evaluate the possible alteration of the vestibulo-ocular reflex (VOR) in patients with horizontal canal benign paroxysmal positional vertigo (h-BPPV) using the video head impulse test (vHIT).
-
Methods
- This was a prospective case-control study of BPPV patients. We include-ed 133 patients with h-BPPV who underwent the vHIT prior to the positioning test. The control group consisted of 76 normal subjects who also underwent the vHIT. The vHIT parameters of gain and asymmetry were assessed, and clinical parameters such as treatment duration, number of canalith reposition maneuvers executed and recurrence rates were evaluated. The VOR and clinical parameters were compared between the h-BPPV and control group. The VOR parameters of h-BPPV canalolithiasis were also compared with those of cupulolithiasis.
-
Results
- The mean age of the patients was 56.5 years and the male to female ratio was 1:2.02. Of the patients, 75 were diagnosed as having the canalolithiasis type of h-BPPV, while the other 58 had the cupulolithiasis type. The mean vHIT gains of the ipsi-lesional horizontal canal plane were 1.13 and 1.15 in the h-BPPV and control group, respectively (p=0.564). However, the asymmetry of the VOR was significantly higher in the h-BPPV than the control group (p=0.013), while the gains and asymmetries of the vHIT in the canalolith and cupulolith types were not significantly different (p=0.454, p=0.826).
-
Conclusion
- The asymmetry of VOR is significantly elevated in the cupulolith type of hBPPV.
-
Keywords: Benign paroxysmal positional vertigo; Otolith; Vestibulo-ocular reflex
-
중심단어: 양성돌발성두위현훈, 이석, 전정안반사
INTRODUCTION
Benign paroxysmal positional vertigo (BPPV) is a clinical disorder characterized by recurrent positional vertigo [1]. BPPV is considered the most common vestibular disease with a prevalence of 10.7–64.0 cases per 100,000 population. The female- to-male ratio of BPPV patients has been reported to range from 2:1 to as much as 3:1 [2].
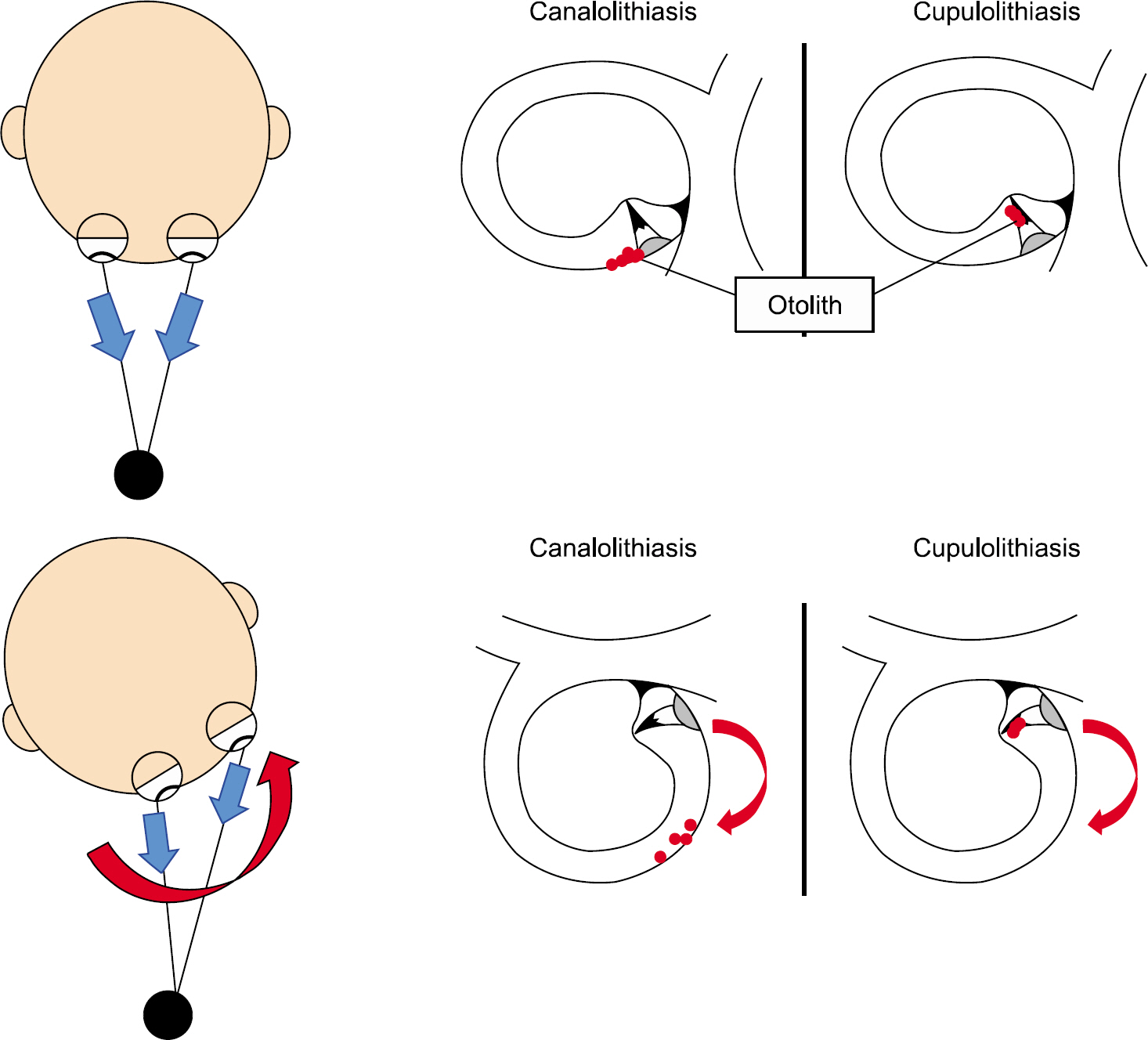
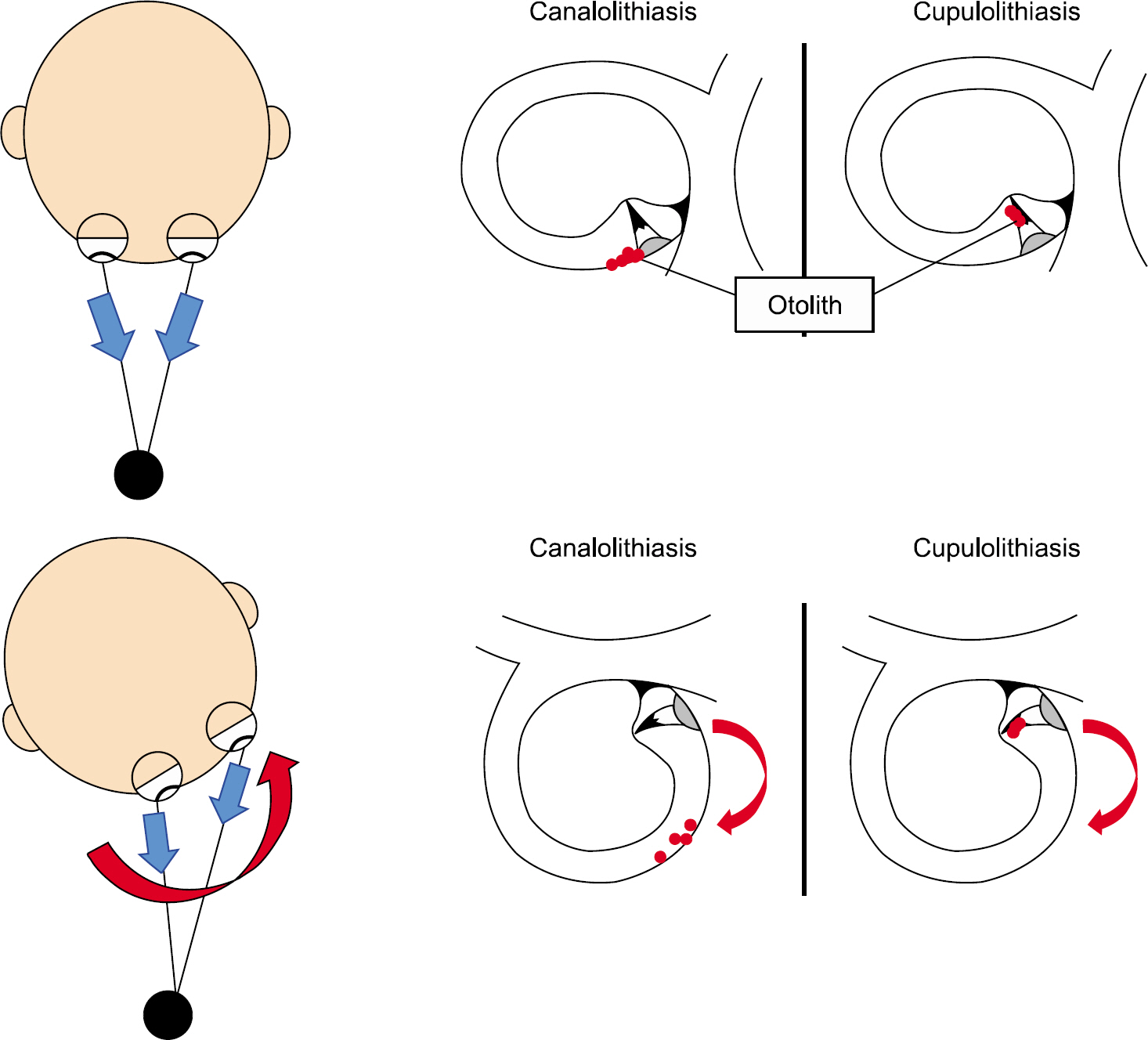
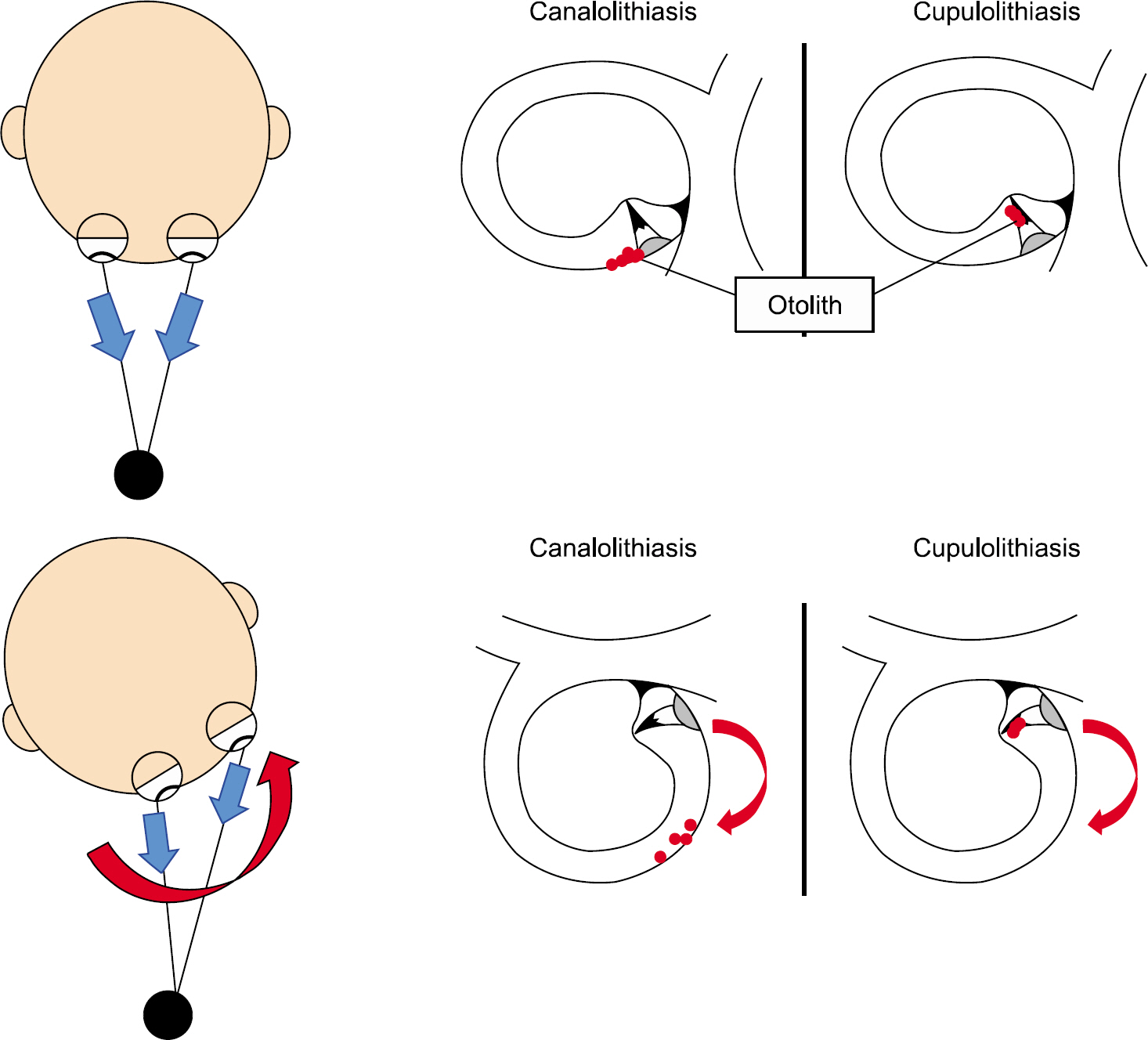
Otoconial debris that dislodges from the utricular macula can precipitate into the semicircular canals [3], and its movement in the endolymph produces push or pull forces on the cupula of the semicircular canal, thereby eliciting excitation or inhi-bition of the corresponding semicircular canals that results in the characteristic nystagmus (Fig. 1) [4]. Therefore, the diag-nosis of BPPV is made by identifying the characteristic positioning nystagmus during the Dix-Hallpike and supine head roll tests [5–7].
Fig. 1.Schematic diagram of the influence of an otolith on the ves-tibular-ocular reflex during rapid head movement (right ear).
The vestibulo-ocular reflex (VOR) is a reflex between the vestibular system and ocular movement that stabilizes images during head movements by producing exquisite eye movements. A left head turn induces excitation of the left horizontal semi-circular canal, followed by excitation of the left vestibular nuclei and inhibition of the right vestibular nuclei. After that, exci-tation of the left oculomotor and right abducens nuclei and leading contraction of the left medial rectus and right lateral rectus muscle cause compensatory eye movement to the right side. The rotational VOR related to the plane of each semi-circular canal stabilizes vision during movement.
A previous study showed that disruption of the VOR in terms of caloric hypoexcitability was frequently identified in BPPV patients, especially in the cupulolithiasis type of horizonal canal BPPV. However, no association between symptom duration and caloric results was detected, probably due to the nonphysiologic nature of the caloric stimulation. Likewise, the authors supposed that the atypical dizziness in BPPV might result from the otolith in the endolymph affecting the flow of endolymph and dis-rupting the VOR. Nowadays, the video head impulse test (vHIT) allows the VOR to be easily measured objectively at physi-ologic stimulation speed [8].
To test this idea, we planned a prospective case-control study using vHIT to evaluate the possible alteration of the VOR in patients with horizontal canal BPPV (h-BPPV).
MATERIALS AND METHODS
1. Patients and Study Design
A prospective, case-control study was conducted in a tertiary referral center. From January 2015 to May 2016, 387 patients with suspected BPPV from clinical history and needing pos-itioning nystagmus tests were eligible for the study. The patients all underwent vHIT tests to evaluate the VOR prior to receiving Dix-Hallpike/Head roll tests to diagnose the specific type of BPPV. After positioning nystagmus, only h-BPPV patients were enrolled in the study and those with anterior canal or posterior canal BPPV were not included. We subdivided the patients into canalolithiasis and cupulolithiasis groups based on their cha-racteristic nystagmus in the positioning test. The patients under-went appropriate canalith reposition maneuvers such as Barbecue maneuver or Gufoni's maneuver depending on their final diagnosis.
We excluded subjects with prior experience of vestibular disorder based on medical history. Patients with recent or chronic ear infections, acute hearing loss, inner ear diseases, and oph-thalmologic problems that interfered with video nystagmo-graphy were not included. In addition, h-BPPV patients with unilateral or bilateral vestibulopathy were excluded based on the results of vHIT gain.
Finally, 133 patients diagnosed with h-BPPV were enrolled. In addition, 76 subjects who completed the vHIT without dizziness-related symptoms were assigned as the control group.
2. Ethics Statement
Written informed consent was obtained from all patients before reviewing their medical records. This investigation was approved by the local ethics review board (Hanyang University Guri Hospital: 2020-02-009) and performed in accordnace with the Declaration of Helsinki and good clinical practice guidelines.
3. Diagnosing Horizontal Canal BPPV
To diagnose BPPV, spontaneous and gaze nystagmus were checked, followed by the Bow and Lean Test to detect the presence of nystagmus and to determine the affected side. The Dix-Hallpike and head roll tests were then performed to identify the affected semicircular canal. h-BPPV was confirmed by observing typical geotropic or ageotropic positional nystagmus during the head roll test. When geotropic nystagmus was observed, the lesion side was indicated by the side showing the stronger nystagmus during the head roll test and the diagnosis was canalolithiasis. In the case of ageotropic nystagmus, the lesion was decided by the direction of the nystagmus and diagnosed as cupulolith. We rigorously enrolled only patients who showed a definite change of direction of nystagmus during the supine head roll tests. Recurrence of BPPV was defined as subjects diagnosed with a further case of BPPV after a symp-tom-free period of 2 weeks or more of follow-up.
4. Video Head Impulse Test
The vHIT test was done to measure the VOR in the hori-zontal canal plane, using an ICS impulse (vHIT GN Otometrics, Denmark). The test was conducted by applying unpredictable manual head impulses of approximately 20° with a mean vel-ocity of 150°/sec and a mean acceleration of 1,000° to 2,500°/ sec in the horizontal plane, with the patients fixing their eyes on a target placed 1 m in front of them. At least 20 adequate impulses were applied to the right and left sides for each test. Parameters such as the gain and asymmetry of the VOR were measured. All procedures were conducted by a professional examiner.
Gain is the ratio of eye movement velocity to head move-ment velocity. Relative gain asymmetry (%) was calculated as the difference between the lower and higher gain divided by the sum of gains multiplied by 100.
Relative gain asymmetry ratio (%)=(Gc-Gi)/(Gc+Gi)×100(Gi=ipsilateral gain, Gc=contralateral gain)
Abnormal vHIT was defined when vHIT was located in the gray range which indicates an inadequate VOR. Results below 0.8 were regarded as abnormal gain.
5. Statistical Analysis
The collected data were exported to IBM SPSS Statistics ver. 19.0 (IBM Co., Armonk, NY, USA) to perform statistical anal-yses. Data are expressed as means±standard deviation (para-metric). Comparisons were made between groups using Student t-test (parametric). Proportions were calculated, using Student t-test and the chi-square test to compare vHIT values between groups. For each test, a statistically significant result was taken as p<0.05.
RESULTS
A total of 133 patients were diagnosed as h-BPPV, 75 with canalolithiasis and 58 with cupulolithiasis. Table 1 presents their demographic characteristics. The mean age was 56.5±12.5 years old; the male to female ratio was 1:2.02, and the right side affected was in 73 patients and the left in 60. The patients underwent an average of 2.2±1.8 sessions of the canalith re-position maneuver, and 29 patients suffered recurrent BPPV (13.9%).
Table 1.Clinical characteristics of horizontal canal benign paroxysmal positional vertigo
|
Characteristic |
Value |
|
No. of patients |
130 |
|
Age (yr) |
56.8±12.4 |
|
Sex, male:female (ratio) |
43:87 (1:2.02) |
|
Side of lesion, right:left |
72:58 |
|
Diagnosis |
|
|
Horizontal canal BPPV |
130 (100) |
|
Canalolithiasis |
73 (56.2) |
|
Cupulolithiasis |
57 (43.8) |
|
No. of CRM |
2.1±1.9 (1–10) |
|
Treatment duration |
6.5±6.4 (1–30) |
|
Recurrence |
16 (12.3) |
The VOR gain was not significantly different in the h-BPPV and control group, whereas the asymmetry on vHIT was sig-nificantly higher in the h-BPPV group (p=0.013). A vHIT gain below 0.8 was seen in 3 patients (2.3%) in the hBPPV group and in 1 patient (1.3%) in the control group (Table 2). In a subgroup analysis, cupulolithiasis of hBPPV showed signifi-cantly elevated asymmetry (p=0.011) (Table 3). Other para-meters were not significantly different. There was also no sig-nificant difference in vHIT gain or vHIT asymmetry between the cupulolithiasis and canalolithiasis groups (Table 4).
Table 2.Comparisons of video head impulse test parameters of the horizontal semicircular canal between horizontal canal BPPV and control
|
|
Horizontal canal BPPV (n=130) |
Control (n=75) |
p-value |
|
vHIT gain |
1.15±0.19 |
1.14±0.19 |
0.781 |
|
vHIT asymmetry |
5.46±5.37 |
4.32±2.81 |
0.048 |
Table 3.Comparisons of video head impulse parameters in the horizontal semicircular canal between each type of h-BPPV (canalolithiasis or cupulolithiasis) and the control group
|
|
Canalolithiasis (n=73) |
Control (n=75) |
p-value |
|
vHIT gain |
1.16±0.24 |
1.14±0.19 |
0.610 |
|
vHIT asymmetry |
4.87±3.41 |
4.32±2.81 |
0.328 |
|
Cupulolitdiasis (n=57)
|
Control (n=75)
|
|
|
vHIT gain |
1.14±0.19 |
1.14±0.19 |
0.377 |
|
vHIT asymmetry |
5.91±6.4 |
4.32±2.81 |
0.042 |
Table 4.Comparisons of vHIT parameters in the horizontal semicircular plane between canalolithiasis and cupulolithiasis
|
|
Canalolithiasis (n=73) |
Cupulolithiasis (n=57) |
p-value |
|
vHIT gain |
1.16±0.24 |
1.14±0.19 |
0.555 |
|
vHIT asymmetry |
4.87±3.41 |
5.91±6.4 |
0.239 |
DISCUSSION
This study assessed a possible alteration of the VOR in h-BPPV using vHIT. The results can be summarized as follows: (1) The asymmetry of the VOR was significantly increased in h-BPPV. (2) Cupulolithiasis of h-BPPV displayed the highest asymmetry, and (3) no decrease of VOR gain was evident in h-BPPV.
The VOR guarantees clear vision during head rotation. The rotational VOR produces a slow phase eye movement that compensates for horizontal, vertical and torsional head rotations. The ordinary rotational VOR compensates perfectly for both the direction and speed of horizontal and vertical head rotations. The eye movements remain well-aligned with the head in the direction of its rolling rotation.
BPPV can be categorized into 2 types, canalolithiasis and cupulolithiasis. “Canalolithiasis” involves free-floating particles within a semicircular canal [9]. Canlolithiasis is mostly due to free-floating debris in the endolymph, which tends to gravitate towards the posterior canal, the most gravity-affected part of the vestibular labyrinth in both upright and supine positions. Once debris enters the posterior canal, the cupula barrier at the end of the canal prevents its exit and it can only prolapse at the end at the ampulla (the common crus) [7]. “Cupulolithiasis” involves particles adherent to the cupula of a semicircular canal [10]. Since particles adhere to the cupula, the vertigo is often severe and persists while the head is in the provoking position. When the head rotates toward the affected side, the cupula undergoes an ampullofugal (inhibitory) deflection causing ageo-tropic nystagmus. Turning the head in the opposite side creates an ampullopetal (stimulatory) deflection, resulting in stronger ageotropic nystagmus [7]. Ageotropic nystagmus is present in about 27% of patients with h-BPPV [11].
The present study was conducted to test the possibility that the presence of otoliths can affect the VOR. Studies have pointed to canal paresis in the caloric test in patients with BPPV by showing that unilateral caloric loss occurs in up to 36% of h-BPPV patients. They also showed that the side with the de-creased caloric response corresponded to the side with the highest-velocity horizontal positional nystagmus [12]. Another study demonstrated reversibility of the hypoexcitability in the caloric test after a liberatory maneuver [13,14].
It has been speculated that cupulolithiasis may affect the cupular deflection due to the weight of otoconia during the rotary chair test. However, the gain and time constant did not differ between cupulolithiasis and canalolithiasis [15]. This suggests that the otolith has little effect on the VOR. However, a recent polot study revealed that gain in the vHIT in the plane of the posterior semicircular canal was reduced in posterior semicircular canal BPPV, suggesting a possible otolithic influence on the VOR in different angle or velocity [2].
The caloric test, rotary chair test, and vHIT can assess the functioning of the VOR in response to different stimulus fre-quencies. The vHIT evaluates frequencies around 2.5 Hz using rapid and short head impulses, whereas the caloric test activates lower frequency bands around 0.003Hz [16]. The rotatory chair test generally evaluates frequencies around 0.01–1 Hz. In daily life, people usually experience head rotation frequencies ranging from 1 Hz to as high as 6 Hz [17]. Since the rotatory chair test and the caloric test cannot reflect the VOR at high fre-quency, these tests do not directly reflect the functional changes of patients' VORs in daily life. Thus, the vHIT test may better reflect the physiologic status of the VOR.
The present study showed that the vHIT gain was not significantly different between h-BPPV and control, whereas the asymmetry of vHIT was significantly elevated in h-BPPV patients. In addition, vHIT gain and asymmetry did not signifi-cantly differ between canalolithiasis and cupulolithiasis.
Interestingly, the asymmetry of vHIT was significantly ele-vated in cupulolithiasis. We assume that the otolith adhering to the cupula may influence the resting state of the cupula making it heavier, and lead to increased gain asymmetry. Ac-cordingly, the distorted input from the semicircular canal may then affect the velocity storage system that enhances VOR per-formance by CNS [18]. However, in canalolithiasis, gain asym-metry is not influenced by the presence of an otolith due to physical factors such as the weight or static friction [19]. Like-wise, the otolith is far from the cupula in canalolithiasis, so it probably cannot affect the VOR gain during head movement.
There are also numerous reports showing frequent occurrence of BPPV on the side of vestibular hypofunction [20,21]. Ab-normal caloric results are frequently seen in BPPV patients even after performing the canalith reposition maneuver [20,22]. It has been postulated that detachment of the otolith from utricle or saccule in BPPV might also have an adverse effect on the trans-itional VOR [23]. Although this study did not include patients with prior experience of vestibulopathy by history, the possible coexistence of vestibulopathy might interfere with interpretation of the results.
There are a few limitations to the present study. We could not perform other vestibular function tests including the caloric test, vestibular evoked myogenic potential, and rotary test, which could provide information on the specific functional status of the vestibular system. In addition, it might have been valuable to compare the result of the vHIT before and after treatment, since this could have provided more direct evidence concerning BPPV's influence on vHIT. In future studies, it would be advisable to examine how vHIT results change after BPPV treatment.
In conclusion, the study showed that the asymmetry of vHIT gain increased in the cupulolith type of hBPPV, thus demon-strating possible alteration of the VOR.
ARTICLE INFORMATION
-
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1. von Brevern M, Radtke A, Lezius F, Feldmann M, Ziese T, Lempert T, et al. Epidemiology of benign paroxysmal positional vertigo: a population based study. J Neurol Neurosurg Psychiatry 2007;78:710–5.ArticlePubMed
- 2. Fallahnezhad T, Adel Ghahraman M, Farahani S, Hoseinabadi R, Jalaie S. Vestibulo-ocular reflex abnormalities in posterior semicircular canal benign paroxysmal positional vertigo: a pilot study. Iran J Otorhinolaryngol 2017;29:269–74.PubMedPMC
- 3. Luis L, Costa J, Vaz Garcia F, Valls-Solé J, Brandt T, Schneider E. Spontaneous plugging of the horizontal semicircular canal with reversible canal dysfunction and recovery of vestibular evoked myogenic potentials. Otol Neurotol 2013;34:743–7.ArticlePubMed
- 4. Brandt T, Steddin S. Current view of the mechanism of benign paroxysmal positioning vertigo: cupulolithiasis or canalolithiasis? J Vestib Res 1993;3:373–82.PubMed
- 5. Strupp M, Brandt T. Peripheral vestibular disorders. Curr Opin Neurol 2013;26:81–9.ArticlePubMed
- 6. Oh SY. Diagnosis of benign paroxysmal positional vertigo. Res Vestib Sci 2013;12:73–8.
- 7. Parnes LS, Agrawal SK, Atlas J. Diagnosis and management of benign paroxysmal positional vertigo (BPPV). CMAJ 2003;169:681–93.PubMedPMC
- 8. Welgampola MS, Taylor RL, Halmagyi GM. Video head impulse testing. Adv Otorhinolaryngol 2019;82:56–66.ArticlePubMed
- 9. Hall SF, Ruby RR, McClure JA. The mechanics of benign paroxysmal vertigo. J Otolaryngol 1979;8:151–8.PubMed
- 10. Schuknecht HF. Cupulolithiasis. Arch Otolaryngol 1969;90:765–78.ArticlePubMed
- 11. Uno A, Moriwaki K, Kato T, Nagai M, Sakata Y. Clinical features of benign paroxysmal positional vertigo. Nihon Jibiinkoka Gakkai Kaiho 2001;104:9–16.ArticlePubMed
- 12. Baloh RW, Jacobson K, Honrubia V. Horizontal semicircular canal variant of benign positional vertigo. Neurology 1993;43:2542–9.ArticlePubMed
- 13. Strupp M, Brandt T, Steddin S. Horizontal canal benign paroxysmal positioning vertigo: reversible ipsilateral caloric hypo-excitability caused by canalolithiasis? Neurology 1995;45:2072–6.ArticlePubMed
- 14. Korres SG, Balatsouras DG, Ferekidis E. Electronystagmographic findings in benign paroxysmal positional vertigo. Ann Otol Rhinol Laryngol 2004;113:313–8.ArticlePubMed
- 15. Kim MT, Choi JE, Lee MY, Jung JY. Can cupulolithiasis affect the time constant or gain of the velocity step test? Res Vestib Sci 2019;18:98–102.ArticlePDF
- 16. Halmagyi GM, Curthoys IS, Cremer PD, Henderson CJ, Todd MJ, Staples MJ, et al. The human horizontal vestibulo-ocular reflex in response to high-acceleration stimulation before and after unilateral vestibular neurectomy. Exp Brain Res 1990;81:479–90.ArticlePubMedPDF
- 17. Park HM, Kim YH, Rhee CK. Active head rotation test in unilateral and bilateral peripheral vestibulopathy. Korean J Otorhinolaryngol-Head Neck Surg 1998;41:856–61.
- 18. Sung KB, Lee TK. Central mechanism of the vestibular-ocular reflex (VOR). Res Vestib Sci 2002;1:56–66.
- 19. Koizuka I, Schor RH, Furman JM. Influence of otolith organs, semicircular canals, and neck afferents on post-rotatory nystagmus. J Vestib Res 1996;6:319–29.ArticlePubMed
- 20. Bi J, Liu B, Zhang Y, Duan J, Zhou Q. Caloric tests in clinical practice in benign paroxysmal positional vertigo. Acta Otolaryngol 2019;139:671–6.ArticlePubMed
- 21. Kim EJ, Oh SY, Kim JS, Yang TH, Yang SY. Persistent otolith dysfunction even after successful repositioning in benign paroxysmal positional vertigo. J Neurol Sci 2015;358:287–93.ArticlePubMed
- 22. Yetişer S, İnce D. Caloric analysis of patients with benign paroxysmal positional vertigo. J Int Adv Otol 2017;13:390–3.ArticlePubMedPDF
- 23. Xu H, Liang FY, Chen L, Song XC, Tong MC, Thong JF, et al. Evaluation of the utricular and saccular function using oVEMPs and cVEMPs in BPPV patients. J Otolaryngol Head Neck Surg 2016;45:12. ArticlePubMedPMC
Citations
Citations to this article as recorded by






 KBS
KBS
 PubReader
PubReader ePub Link
ePub Link Cite
Cite


